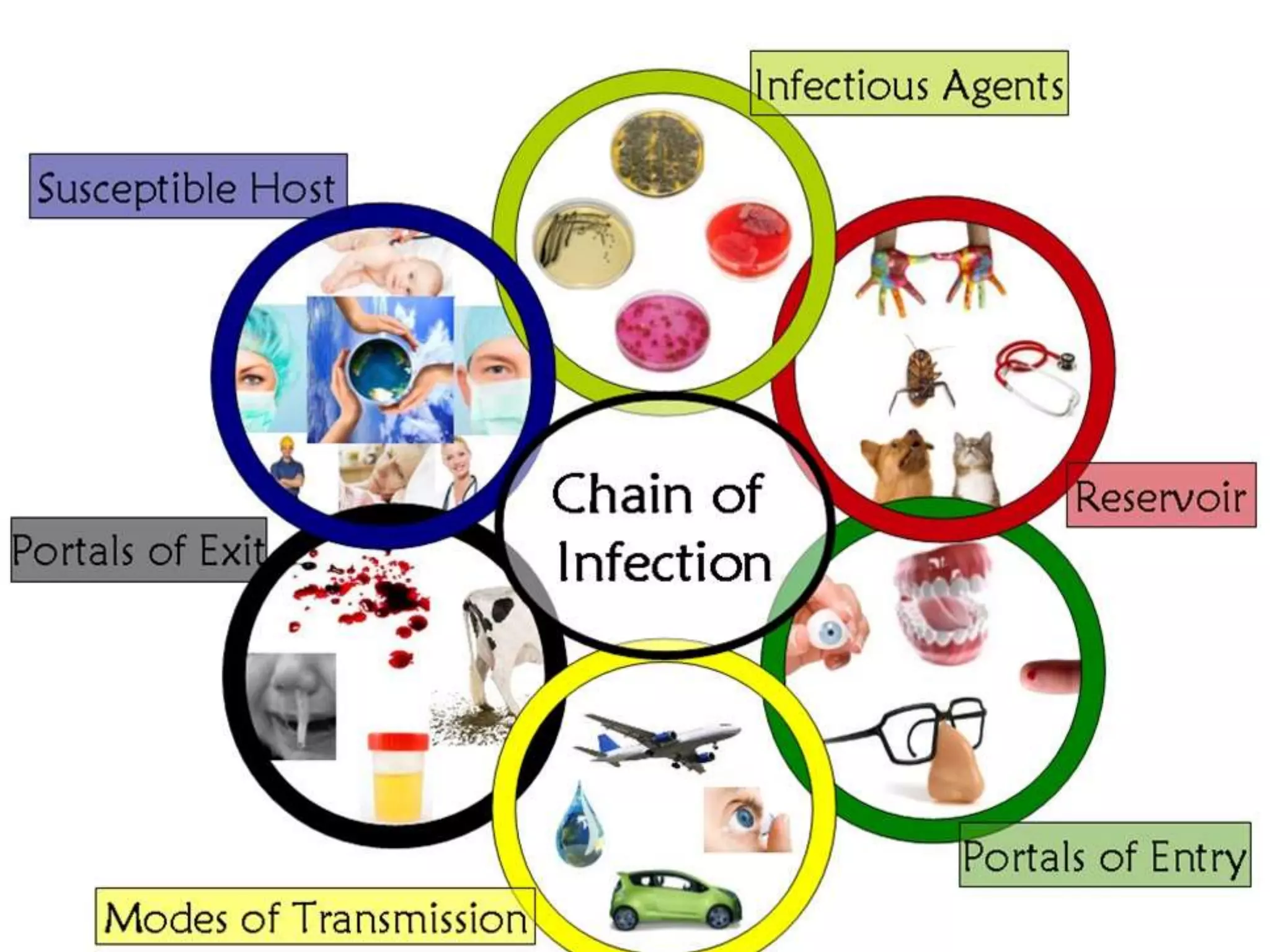
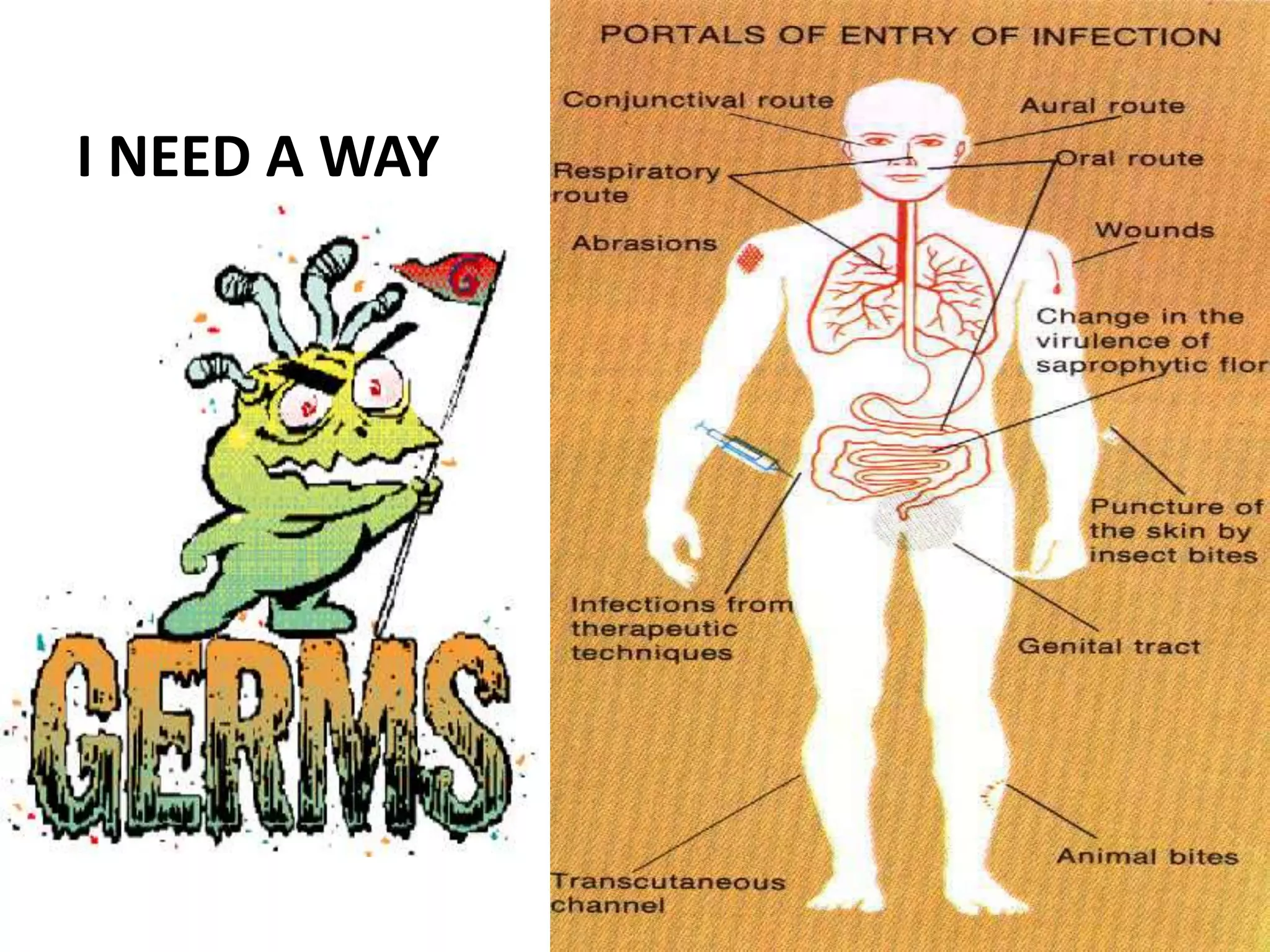
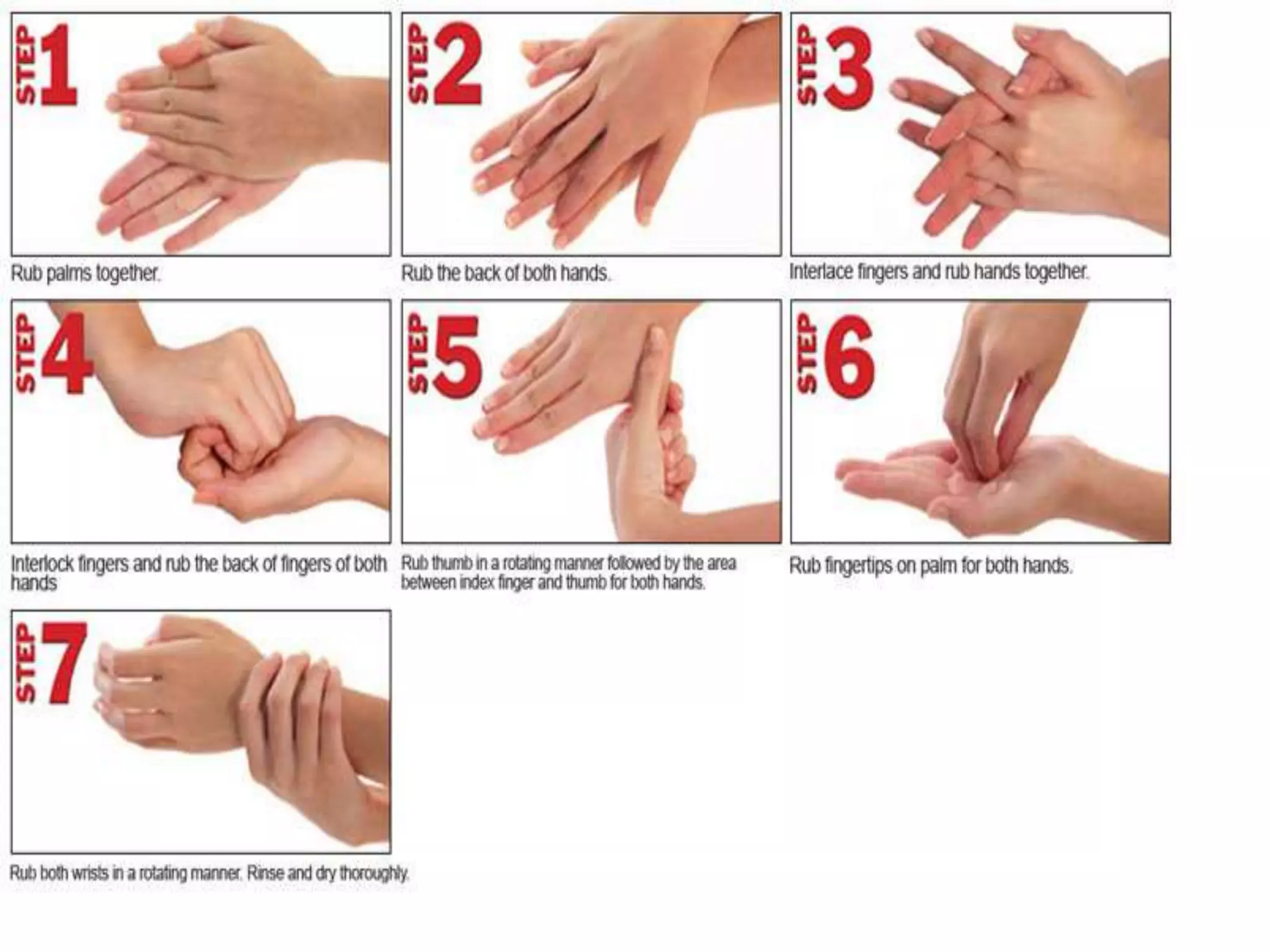
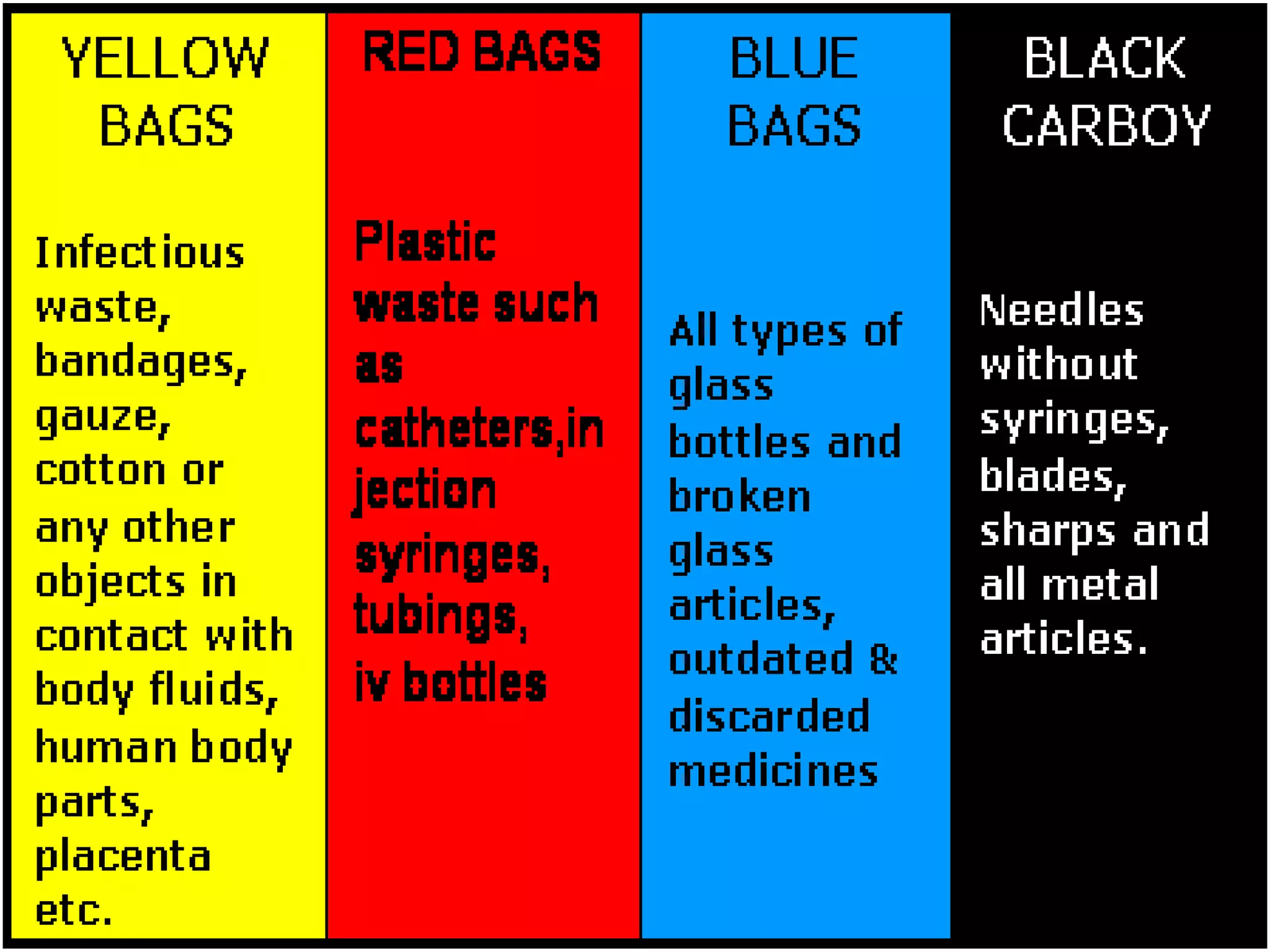
An infection occurs when pathogens invade the body and reproduce, potentially causing disease. Microorganisms are transmitted through body fluids, direct contact, droplets, and contaminated surfaces. Portals of entry include mucous membranes and breaks in the skin. Hospitals present increased infection risks due to patients' health issues, invasive procedures, and virulent pathogen strains. Standard precautions like hand washing, personal protective equipment, sharp handling protocols, and waste management can reduce transmission when applied consistently. Staff education also helps prevent the spread of infections.