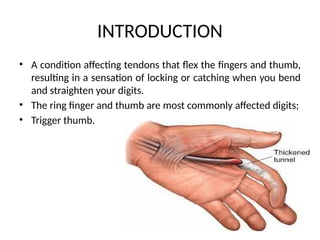
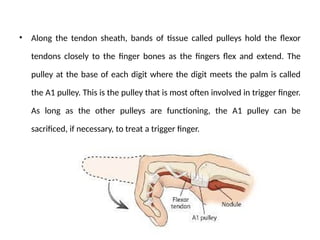
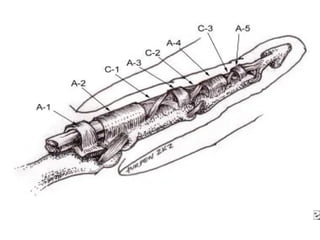
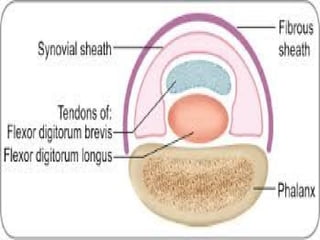
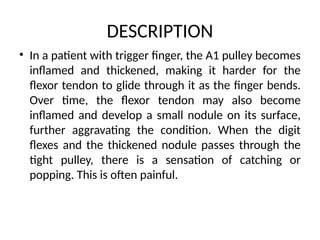
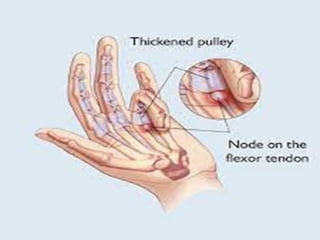
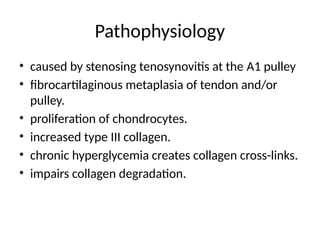
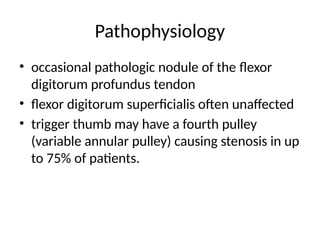
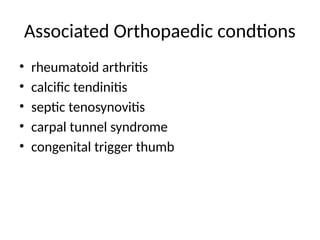
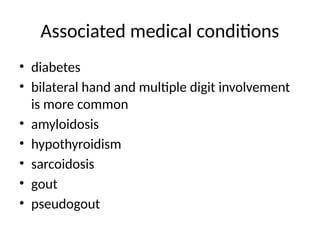
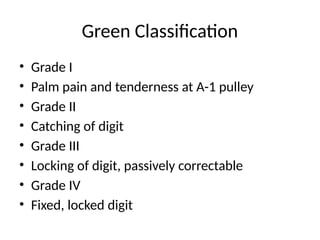
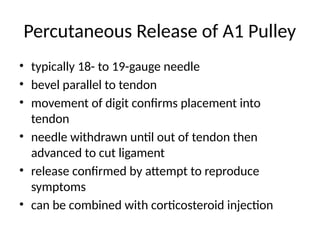
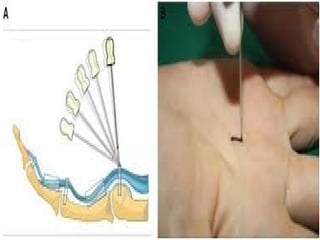
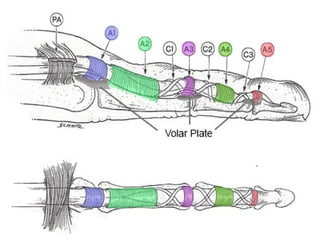
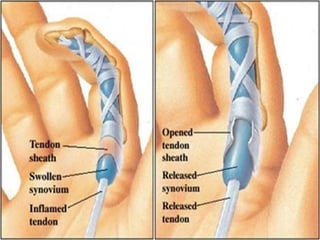
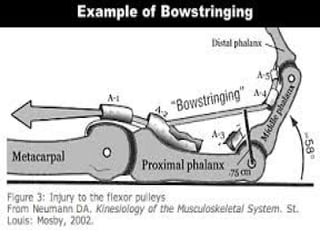
Trigger finger, or stenosing tenosynovitis, is a condition where flexor tendons in fingers lock or catch due to an inflamed A1 pulley, commonly affecting the ring finger and thumb. Symptoms include pain, clicking, and locking of the finger, often exacerbated by conditions like diabetes and rheumatoid arthritis. Management options range from splinting and NSAIDs to corticosteroid injections and possible surgical release if conservative treatments fail.