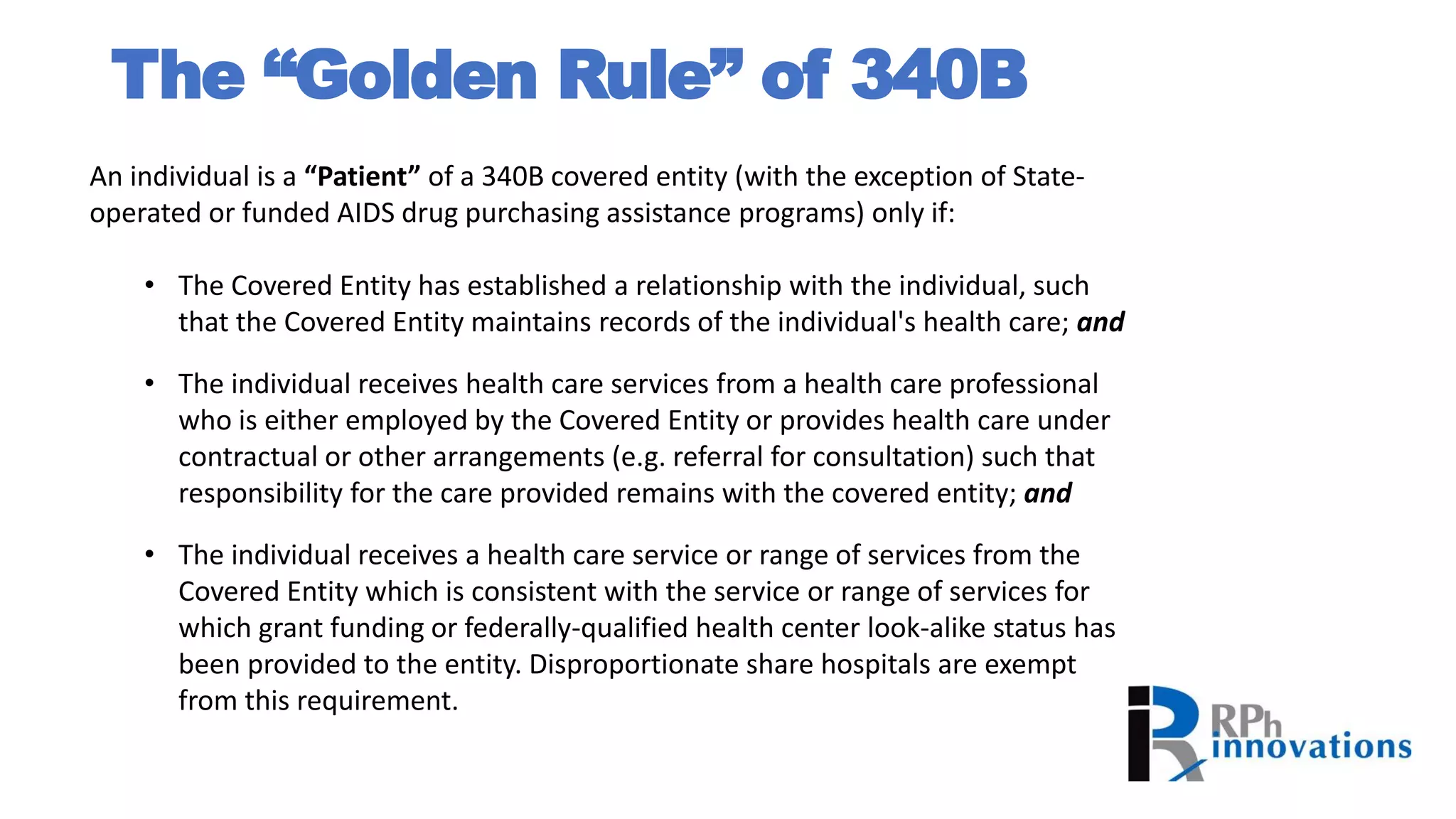
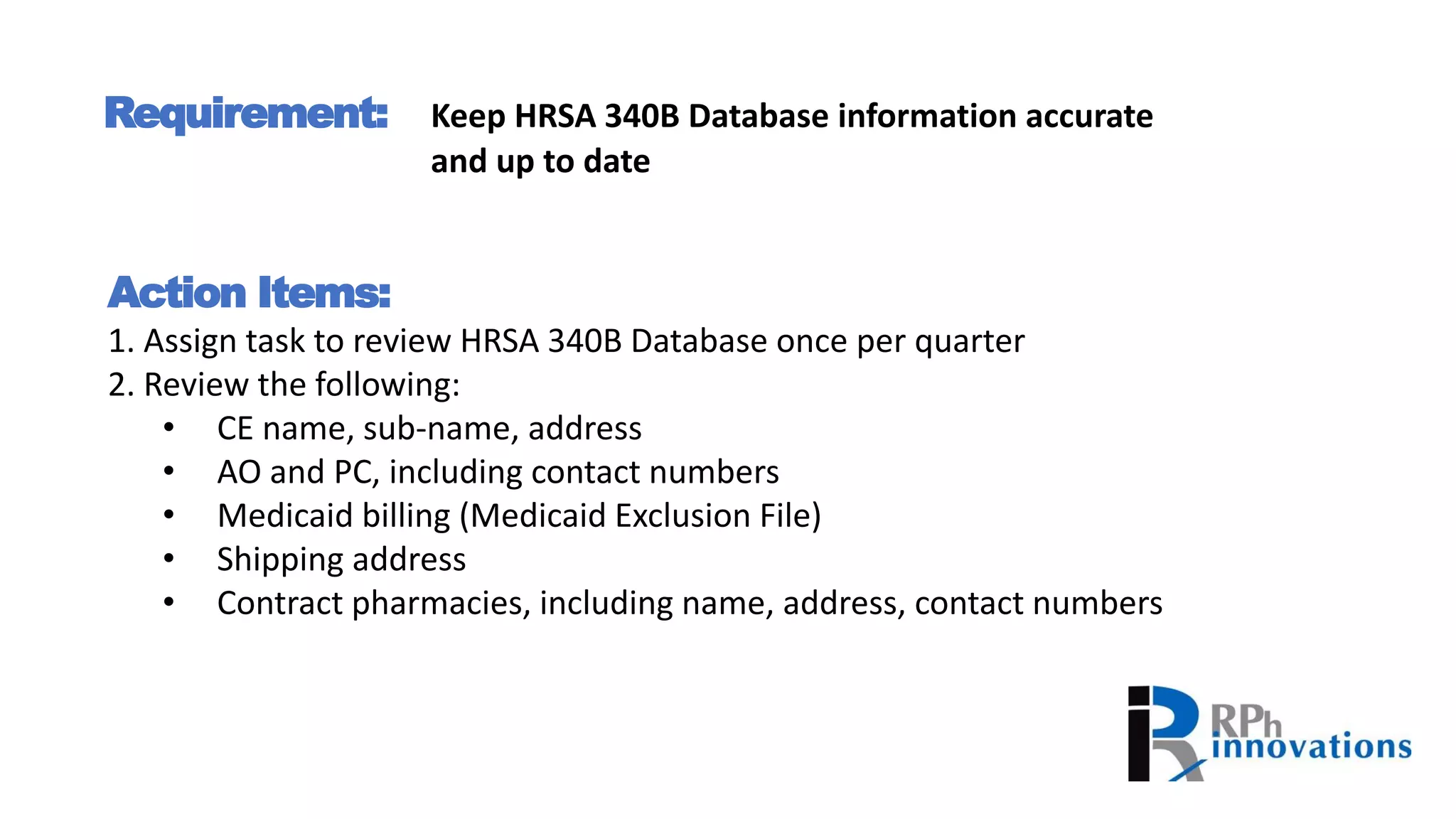
The document provides guidance on complying with 340B program requirements by taking specific action items, such as keeping HRSA 340B database information accurate and up-to-date, preventing diversion of drugs to ineligible patients, preventing duplicate discounts, and preparing for potential audits by maintaining thorough documentation and policies and procedures. Non-compliance can result in findings during HRSA audits, so covered entities must understand eligibility rules, establish data sharing processes, and conduct regular self-audits to ensure only eligible patients and locations are utilizing 340B discounted drugs.