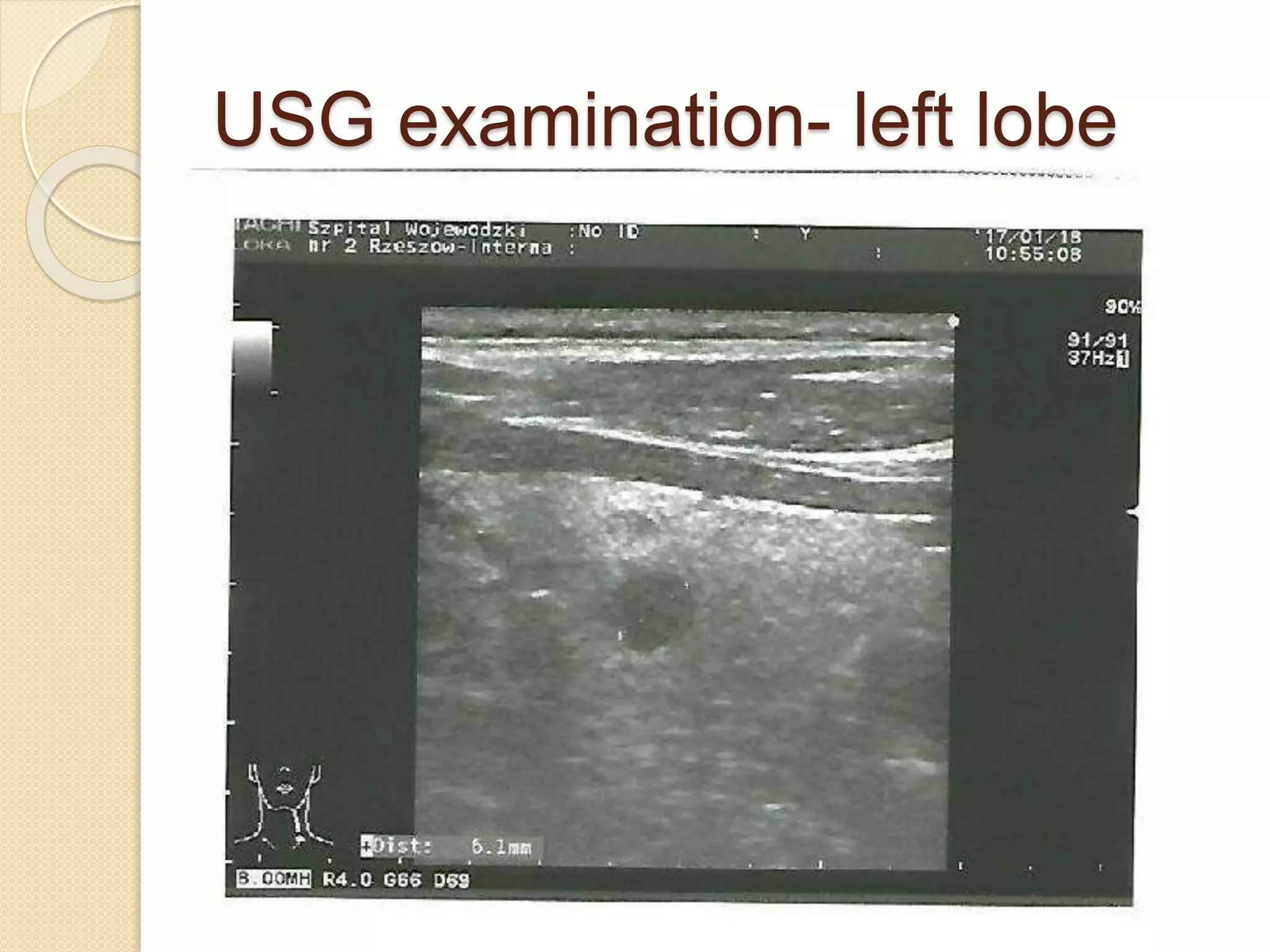
This case report describes a 76-year-old male patient diagnosed with Marine-Lenhart syndrome. The patient had a history of Graves' disease treated with antithyroid drugs. Tests showed suppressed TSH levels and the patient was referred to an endocrinology department. Exams including ultrasound and scintigraphy revealed the patient had Graves' disease along with a hyperactive nodule in the thyroid, consistent with Marine-Lenhart syndrome. The patient was treated with antithyroid drugs followed by radioactive iodine therapy. Follow up showed improvement of hyperthyroidism symptoms. Marine-Lenhart syndrome is a rare cause of hyperthyroidism where a patient has Graves' disease concurrently with a hyperfunctional thyroid nodule.