This document discusses thyroid disorders, including hypothyroidism. Some key points:
- Hypothyroidism affects 1-5 per 1000 live births and is a common cause of preventable mental retardation in children.
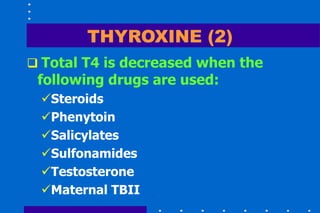
- It can be congenital or acquired, with causes including iodine deficiency, autoimmune thyroiditis, and medications.
- Symptoms include constipation, feeding problems, slow growth, and delayed development.
- Diagnosis involves blood tests showing low thyroid hormones and high TSH. Treatment is lifelong thyroid hormone replacement therapy.
- Early diagnosis and treatment is important for normal development and intelligence.