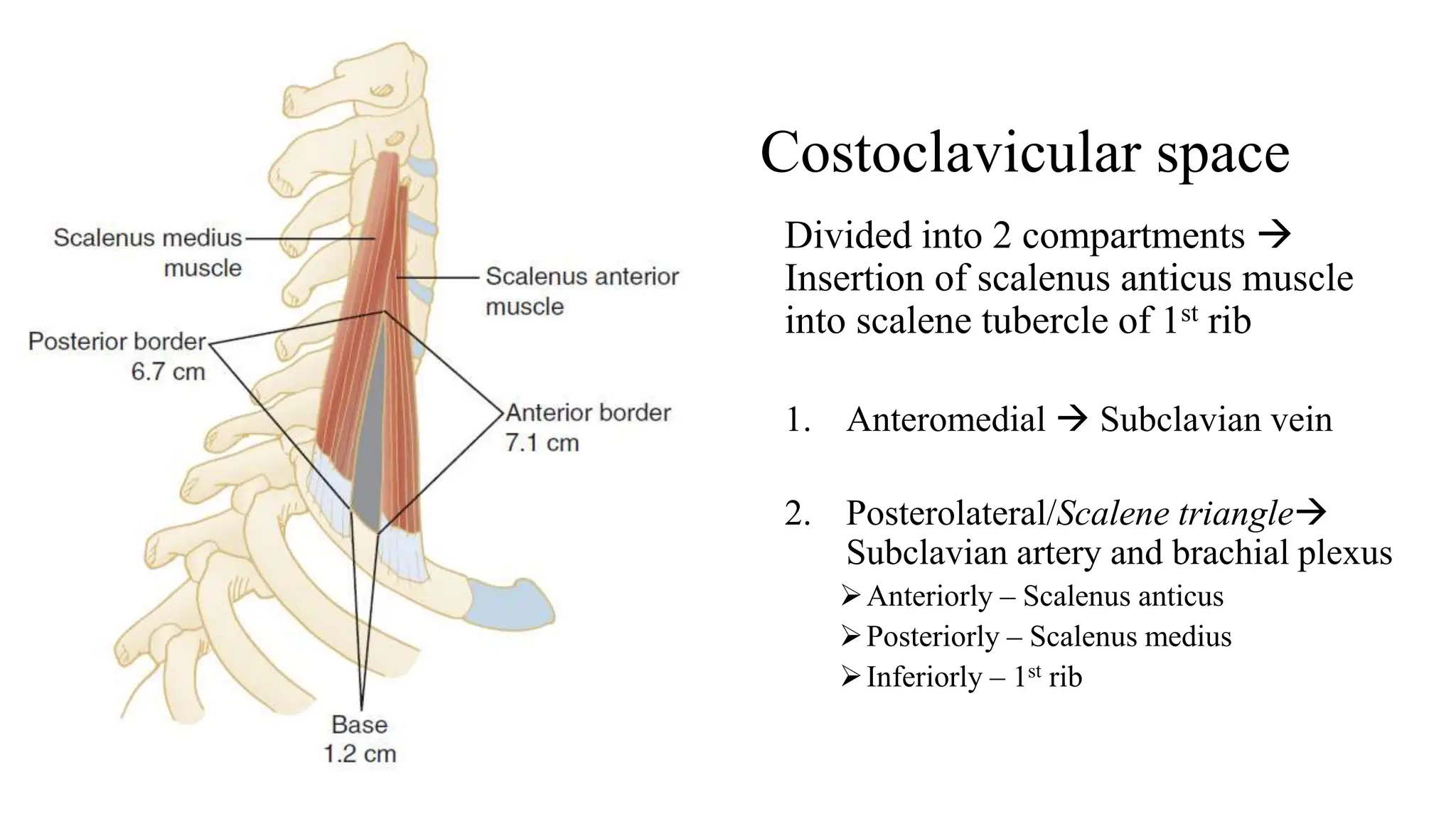
Thoracic outlet syndrome refers to compression of the brachial plexus and subclavian vessels at the thoracic outlet. It has several potential causes including abnormalities of the first rib, scalene muscles, clavicle, and pectoralis minor muscle. Symptoms can be neurogenic like pain, paresthesia and muscle atrophy, or vascular such as coldness, weakness and arterial insufficiency. Diagnosis involves physical exam, imaging, and nerve conduction studies. Treatment ranges from conservative physiotherapy to surgical resection of compressive structures like the first rib via various approaches depending on the type and severity of thoracic outlet syndrome.