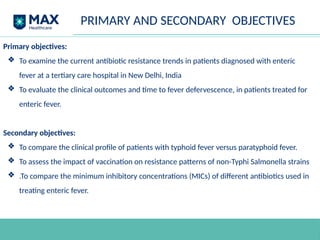
The document presents a study on evolving resistance patterns to antibiotics in enteric fever, specifically focusing on cases in a tertiary care hospital in New Delhi, India. It outlines the increasing resistance of Salmonella enterica serotypes, including multidrug resistance and treatment failures, while highlighting the need for localized resistance data to develop effective treatment strategies. The study also aims to analyze current resistance patterns and clinical responses to antibiotics in enteric fever patients to enhance management and inform public health policies.

![MATERIALS AND METHODS
• Study Area
Present study will be conducted in patients admitted in Medical ward and
ICU of Max Super Speciality hospital , Saket, New Delhi.
• Study Design
Prospective Observational study.
• Study Duration
From approval of Ethical Committee till completion of sample size [1 year]
• Study Population
Study will include patients admitted in medical ward and ICU of Max Super
Specialty Hospital, Saket, New Delhi and :
❏ Inclusion and exclusion criteria will be applied to the patients admitted
with enteric fever.
❏ Informed consent will be obtained from eligible patients.](https://image.slidesharecdn.com/thesisprotocolpptarnav-240912082735-c4ac0f62/85/Thesis-Protocol-PPT-arnav-dengue-typhoid-pptx-17-320.jpg)
![CONSENT FORM
STUDY TITLE: “Evolving Resistance Patterns and Clinical Response to
Antibiotics in Enteric Fever: A Tertiary Care Hospital Study in New Delhi,
India”
Patient’s Name:
Age/Sex:
1. I confirm that I have read and understood the information sheet for the above study and have
had the opportunity to ask questions.[ ]
2. I understand that my participation in the study is voluntary and that I am free to withdraw at
any time, without giving any reason, without my medical care or legal rights being affected. [ ]
3. I understand that the Ethics Committee and the regulatory authorities will not need my
permission to look at my health records both in respect of the current study and any further
research that may be conducted in relation to it, even if I withdraw from the trial. I agree to
this access. However, I understand that my identity will not be revealed in any information
released to third parties or published. [ ]
4. I agree not to restrict the use of any data or results that arise from this study provided such a
use is only for scientific purpose(s). [ ]
5. I agree to take part in the above study. [ ]](https://image.slidesharecdn.com/thesisprotocolpptarnav-240912082735-c4ac0f62/85/Thesis-Protocol-PPT-arnav-dengue-typhoid-pptx-36-320.jpg)