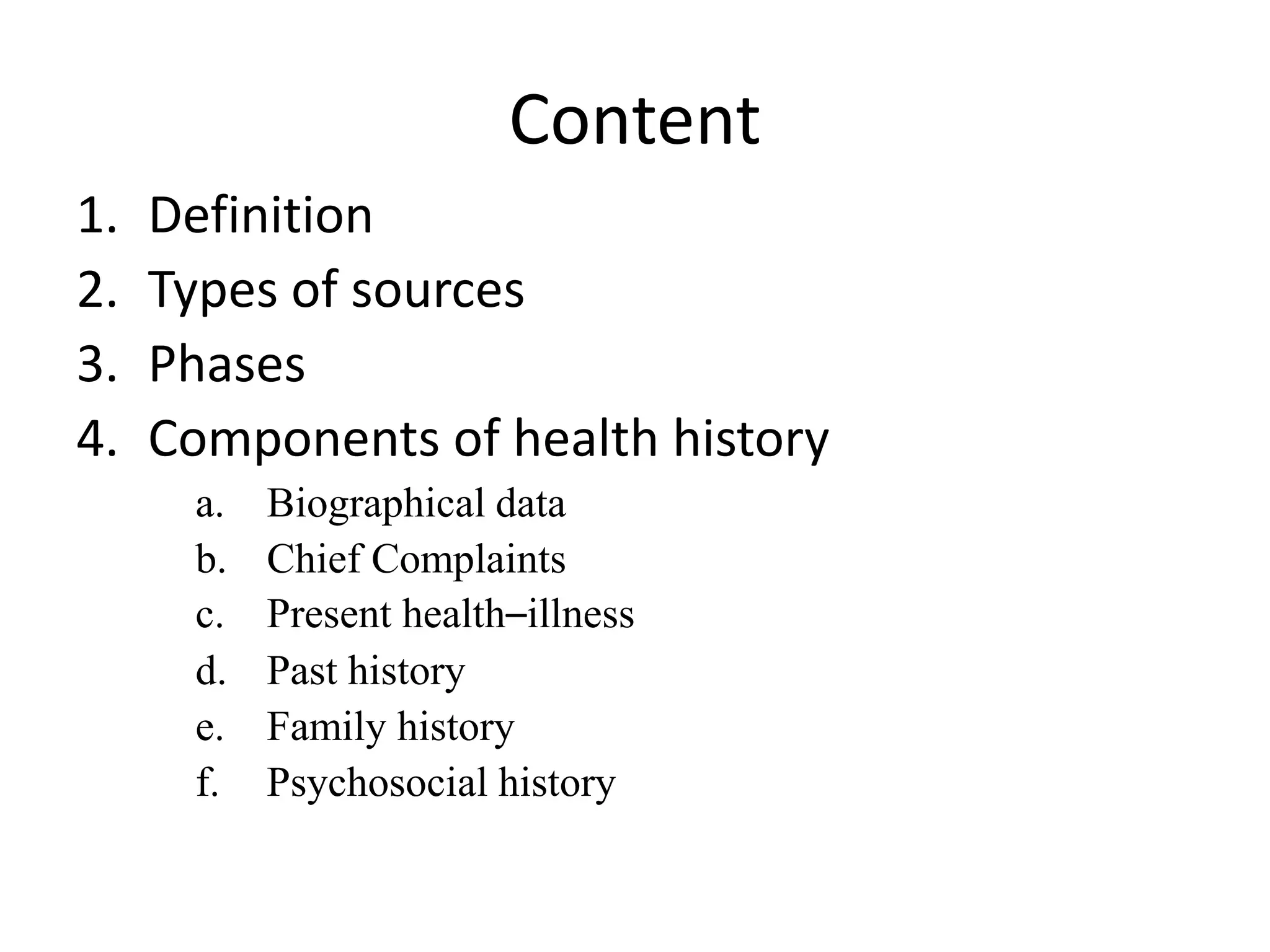
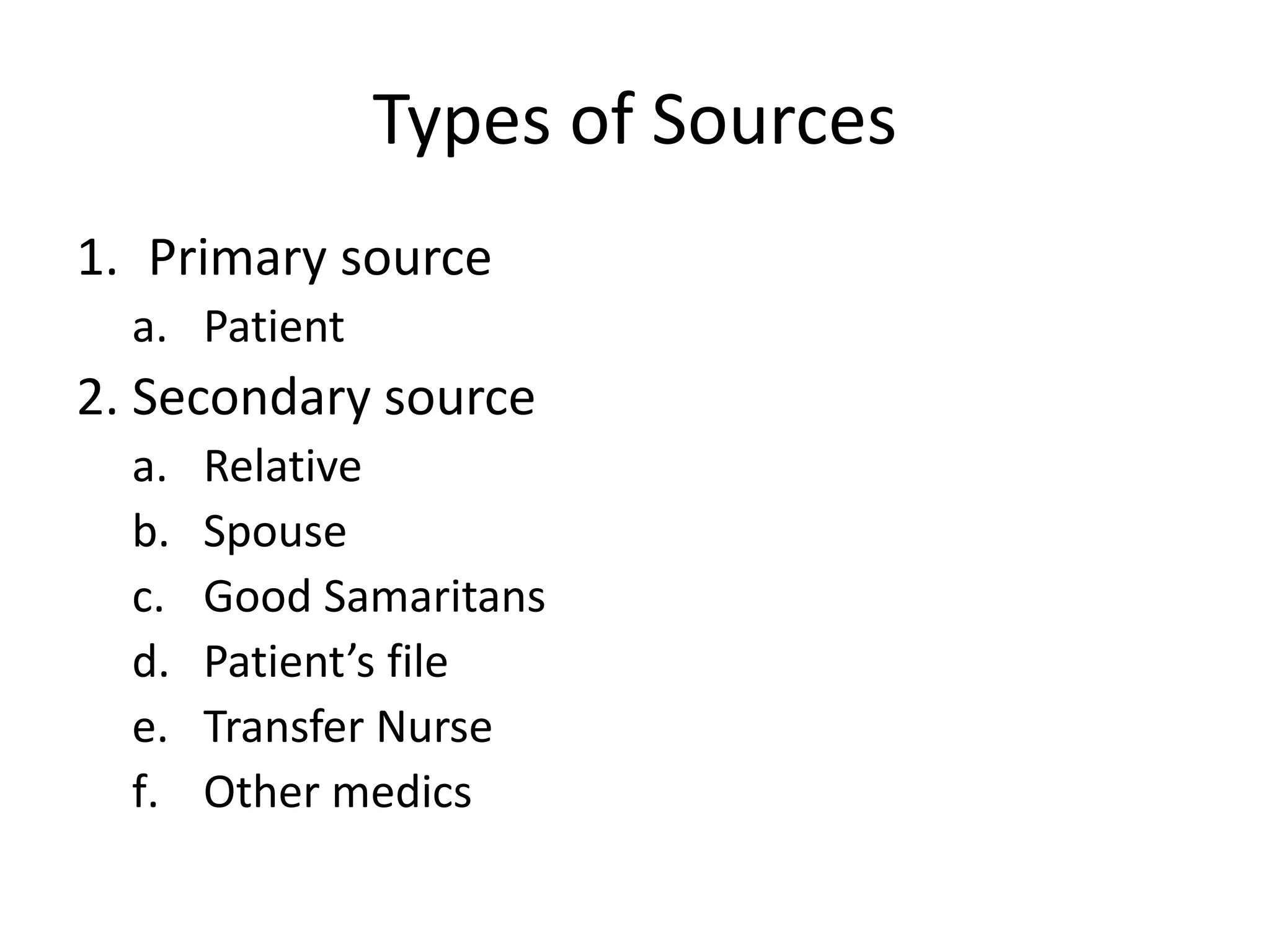
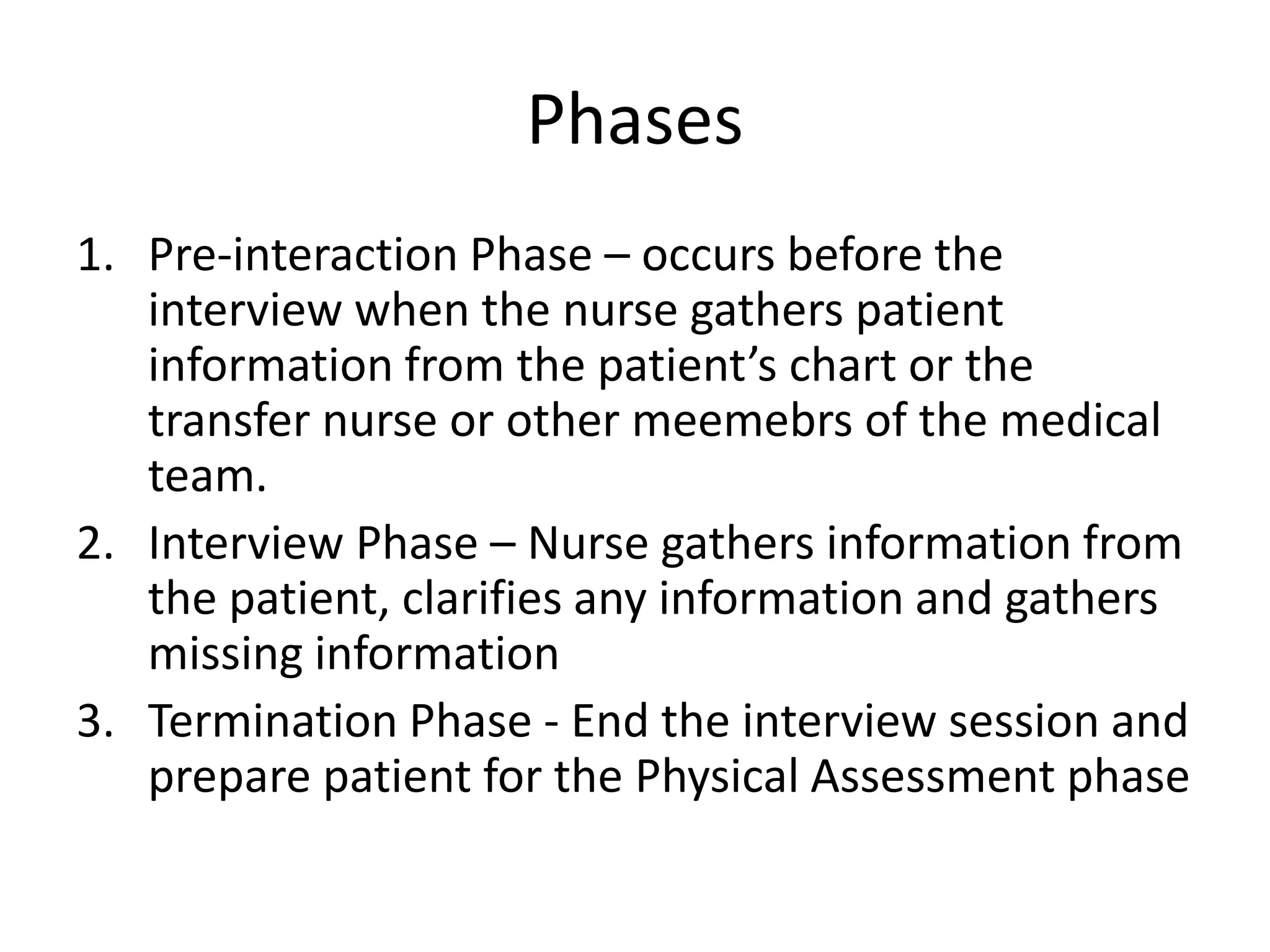
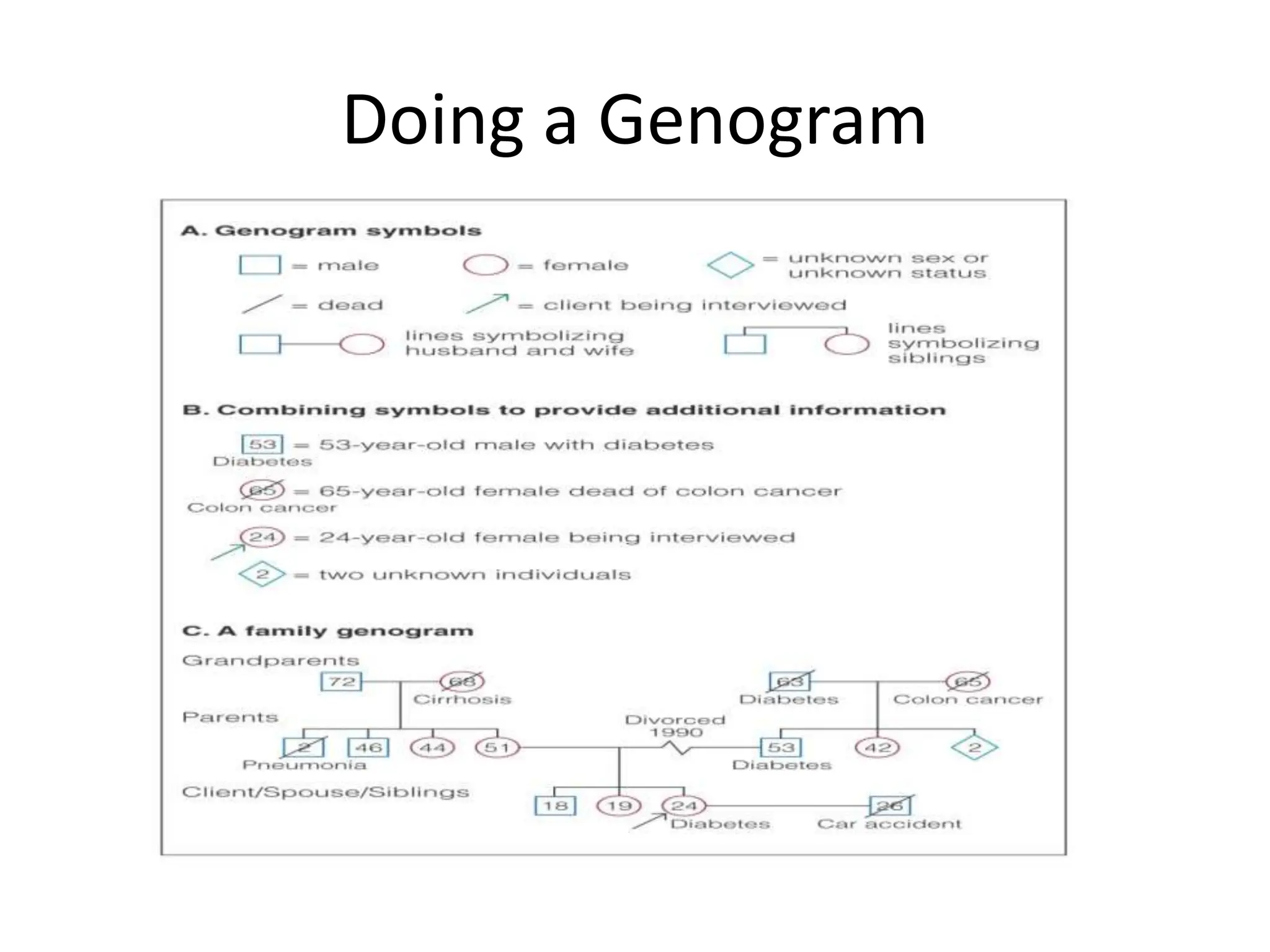
The document outlines the importance of subjective data in health history, which is relevant information provided by patients or their families for healthcare planning. It details the types of sources (primary and secondary), phases of the data collection process (pre-interaction, interview, termination), and the key components of health history including biographical data, chief complaints, and psychosocial history. Additionally, it emphasizes the significance of thorough historical context in understanding a patient's current health status and planning appropriate care.