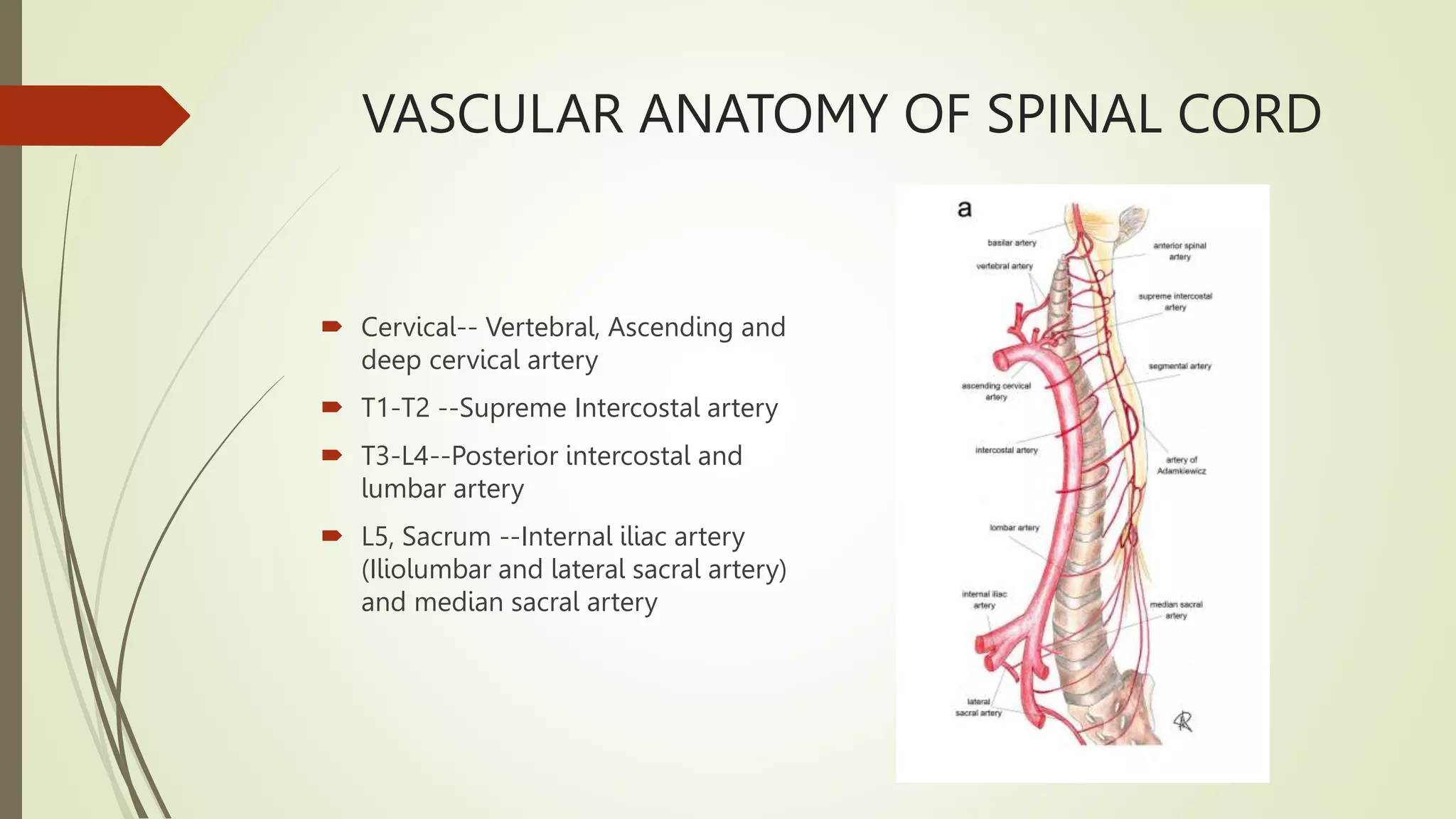
The document provides an extensive overview of spinal cord vascular syndrome, including its diagnosis, clinical presentation, and treatment options. It discusses the vascular anatomy of the spinal cord, various types of arterial and venous ischemia, and the pathophysiology behind these conditions. Additionally, it outlines the investigations required for diagnosis and the management strategies for different types of spinal vascular malformations and hemorrhages.