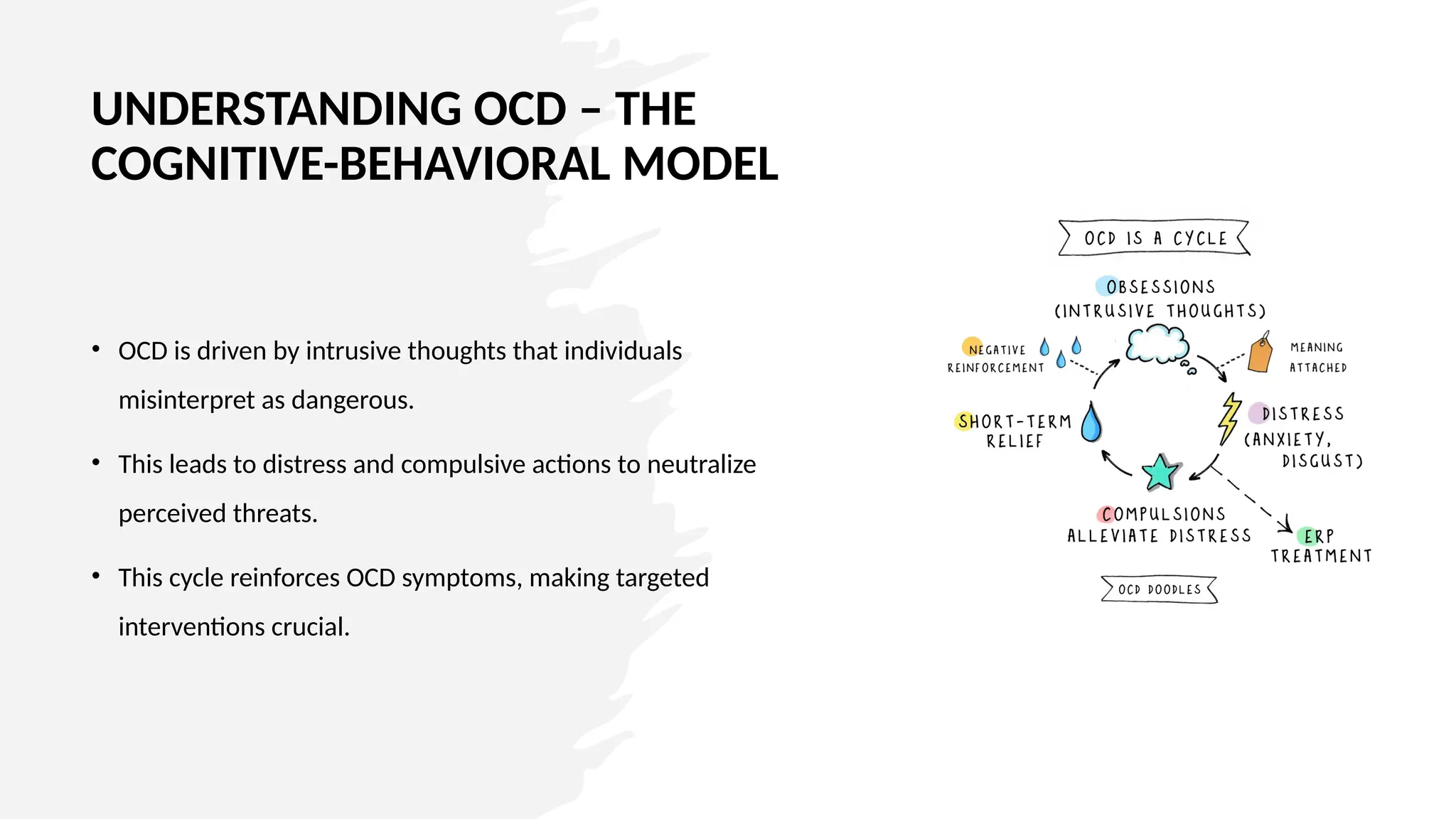
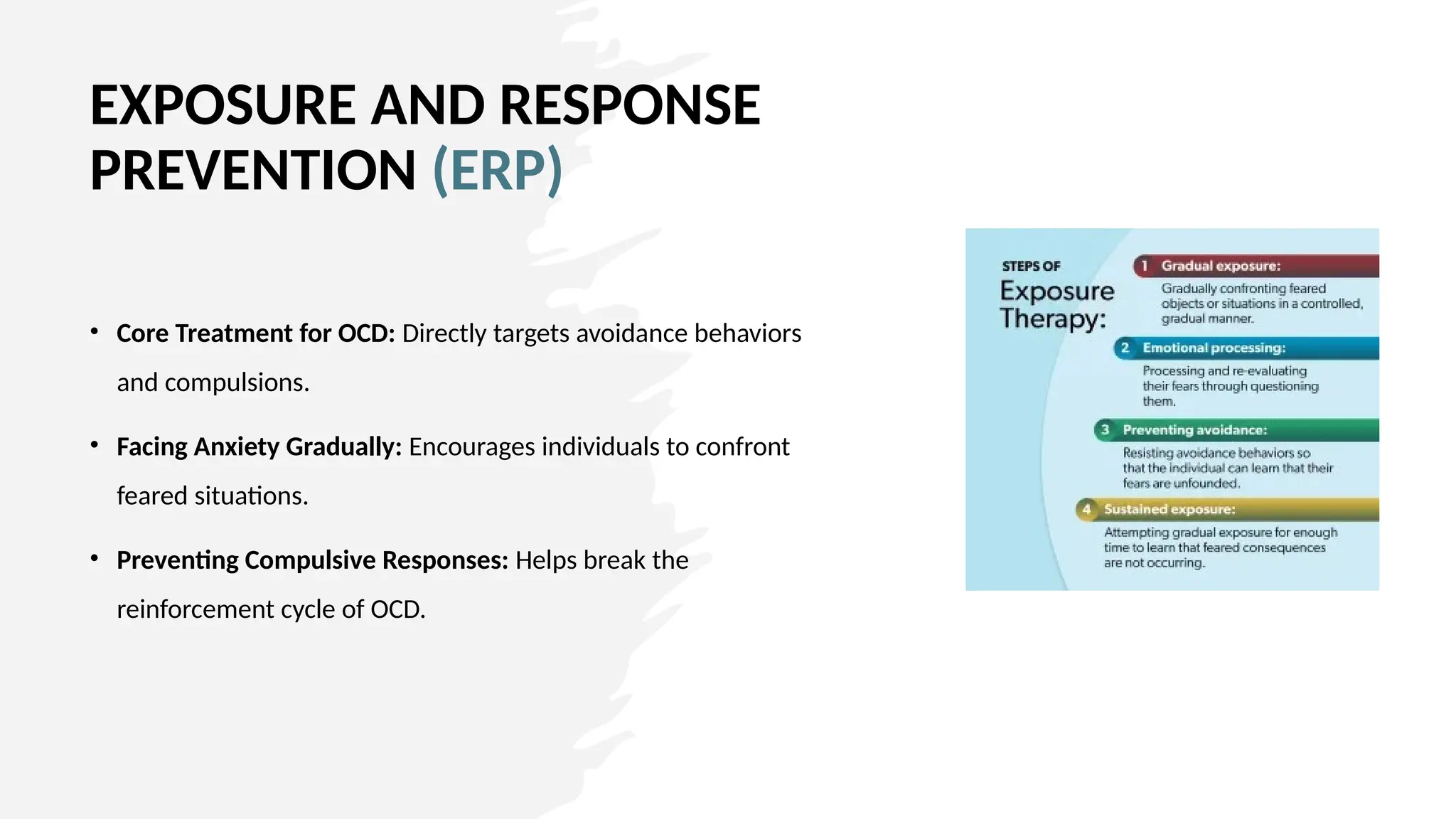
Solution for OCD requires a multifaceted approach that empowers individuals with effective strategies to manage their symptoms. Evidence-based psychological interventions such as CBT, ERP, mindfulness, behavioral techniques, and lifestyle modifications provide robust frameworks for sustained recovery.
At Emotion Of Life, advocating for these non-medication solutions enhances patient autonomy, reduces distress, and fosters resilience. Encouraging individuals to integrate these approaches into their daily lives lead to meaningful improvements in their mental well-being, empowering them to regain control and live fulfilling lives free from the constraints of OCD.