The document provides an overview of the anatomy, physiology, and pathologies of the small intestine. It discusses the following key points:
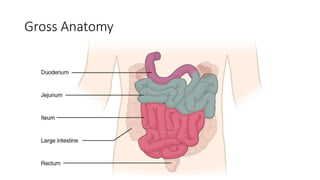
- The small intestine is responsible for digestion and absorption. It starts at the pylorus and ends at the ileocecal valve, measuring around 7 meters long.
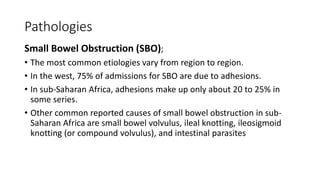
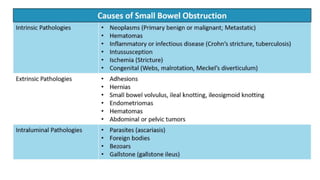
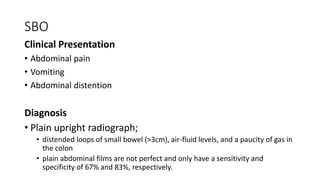
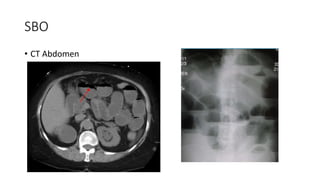
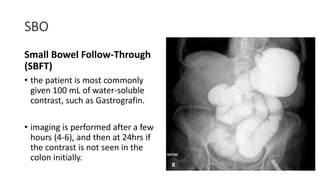
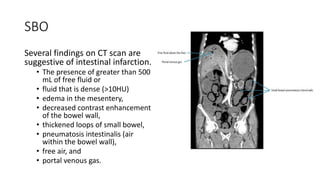
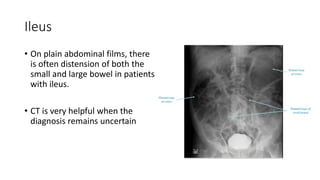
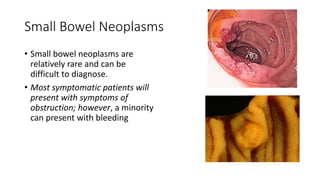
- Common pathologies include small bowel obstruction, which can be diagnosed using imaging like CT scans, and ileus, which results in impaired motility.
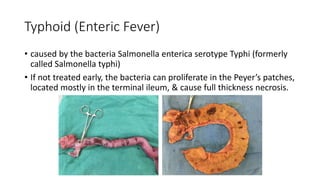
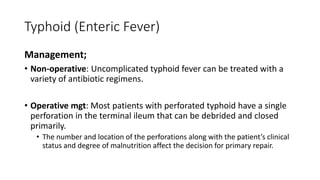
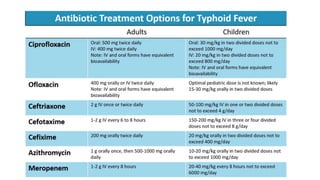
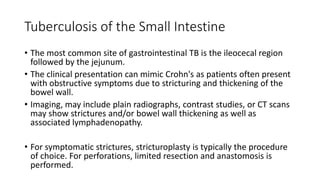
- Infectious diseases like typhoid fever and tuberculosis can also affect the small intestine. Typhoid is caused by Salmonella and can lead to perforation of the ileum if untreated.