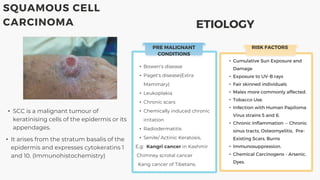
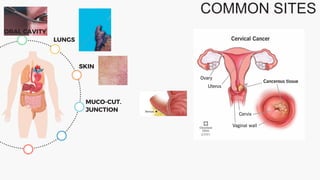
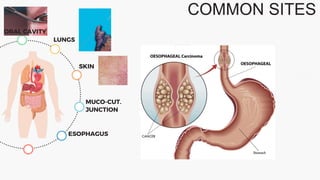
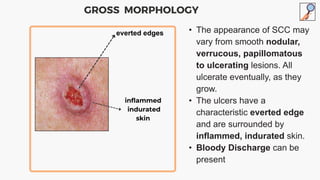
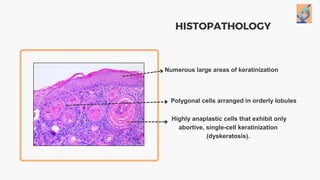
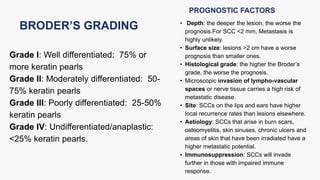
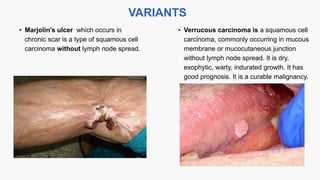
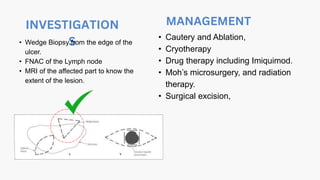
The document outlines various types of skin tumors, including benign and malignant forms such as squamous cell carcinoma (SCC) and its risk factors, etiology, and characteristics. It discusses the prognosis based on depth, size, histological grade, and other factors influencing metastasis and treatment options including surgical excision, radiation therapy, and chemotherapy. Additionally, it highlights the importance of Moh's microsurgery for critical cosmetic sites and poorly differentiated tumors.