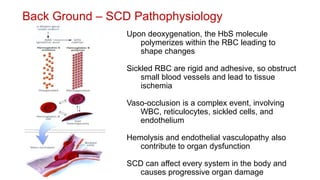
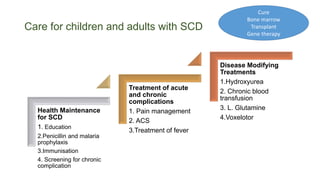
The document outlines comprehensive care for sickle cell disease (SCD), focusing on pathophysiology, management of acute complications, and the use of hydroxyurea. SCD affects a significant number of infants, especially in sub-Saharan Africa, with a high mortality rate before age five, necessitating preventive measures, education, and treatment strategies. Management includes pain relief, screening for complications, and the introduction of disease-modifying treatments such as hydroxyurea, which has shown to effectively reduce pain episodes and complications.