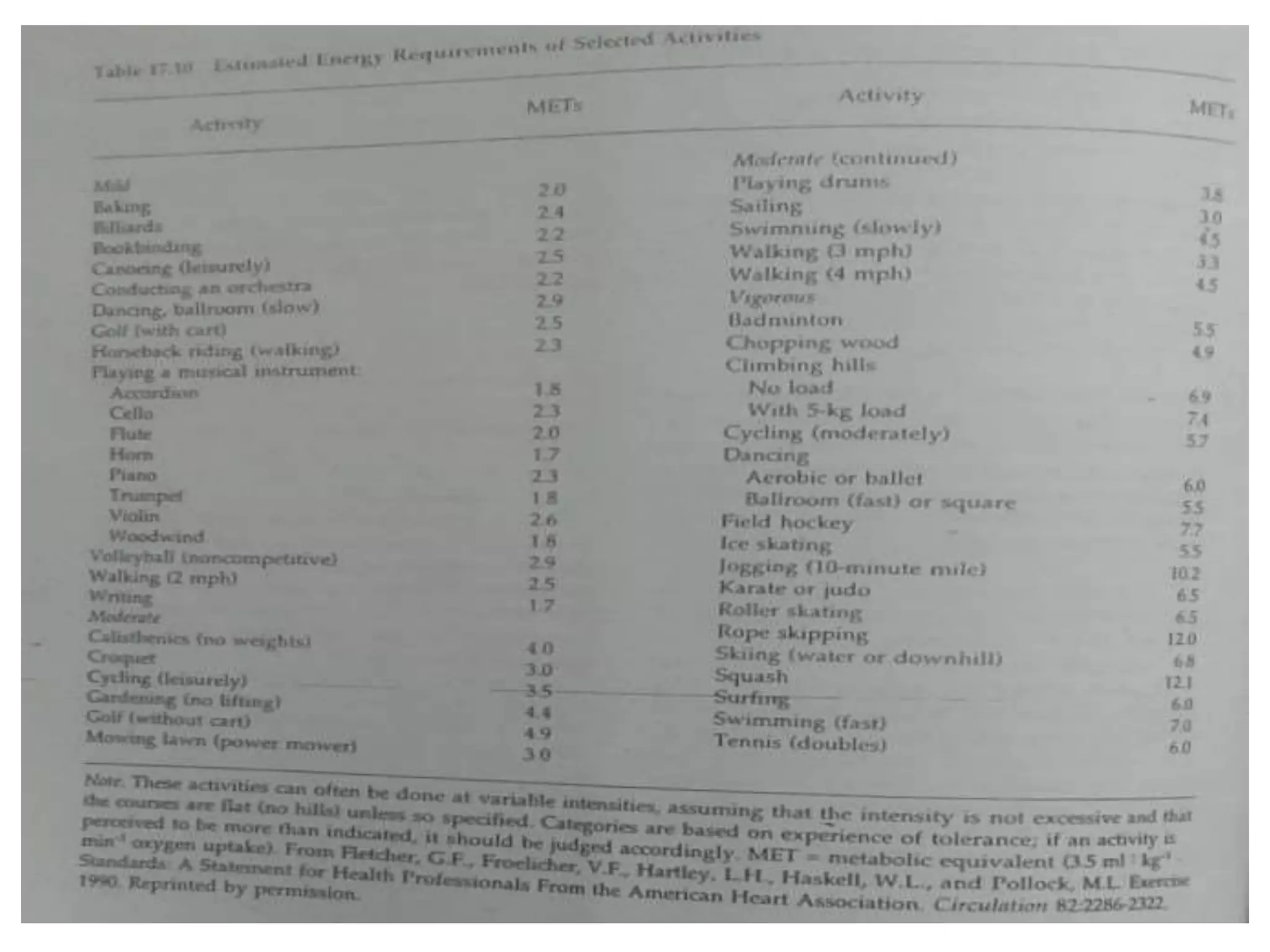
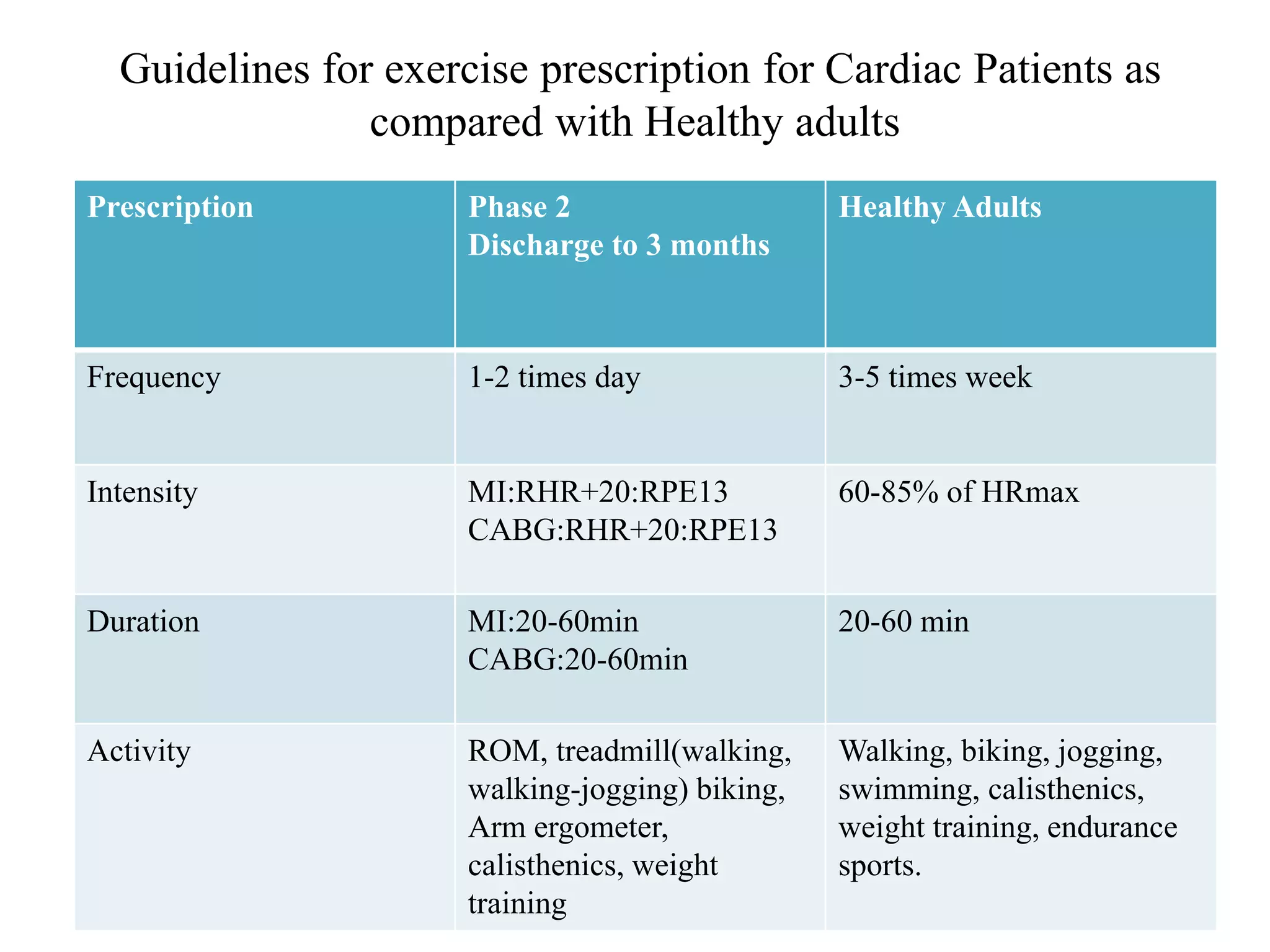
This document provides guidelines for home-based and outpatient cardiac rehabilitation programs. It recommends that cardiac rehabilitation plans be individually tailored and last up to one year. Phase 2 programs should commence within 3 weeks of discharge and focus on improving functional capacity and lowering cardiovascular risk factors. Outpatient programs are an important part of rehabilitation and should begin after discharge. Exercise prescriptions should determine intensity using heart rate, perceived exertion scales, metabolic equivalents or anaerobic thresholds. Frequency and duration of training should gradually increase over weeks. Recommended modes of training include walking, cycling, strength training, and circuit training.