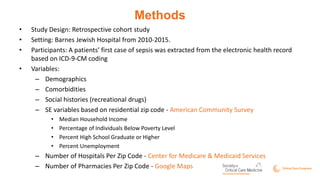
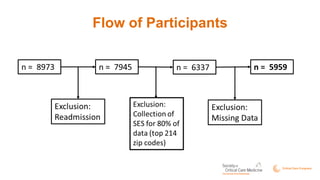
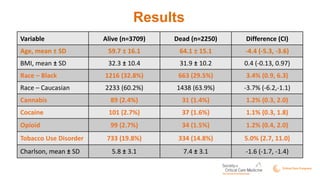
This study examined the influence of social, socioeconomic, and medical histories on sepsis-related mortality. The study retrospectively analyzed data from over 5,000 patients with sepsis from 2010-2015 at Barnes Jewish Hospital. Contrary to expectations, African American patients, those with a history of recreational drug use, and those from zip codes with higher incomes and education levels had lower mortality. Further analysis is needed to understand these unexpected results and identify relationships between pre-admission variables and in-hospital mortality.