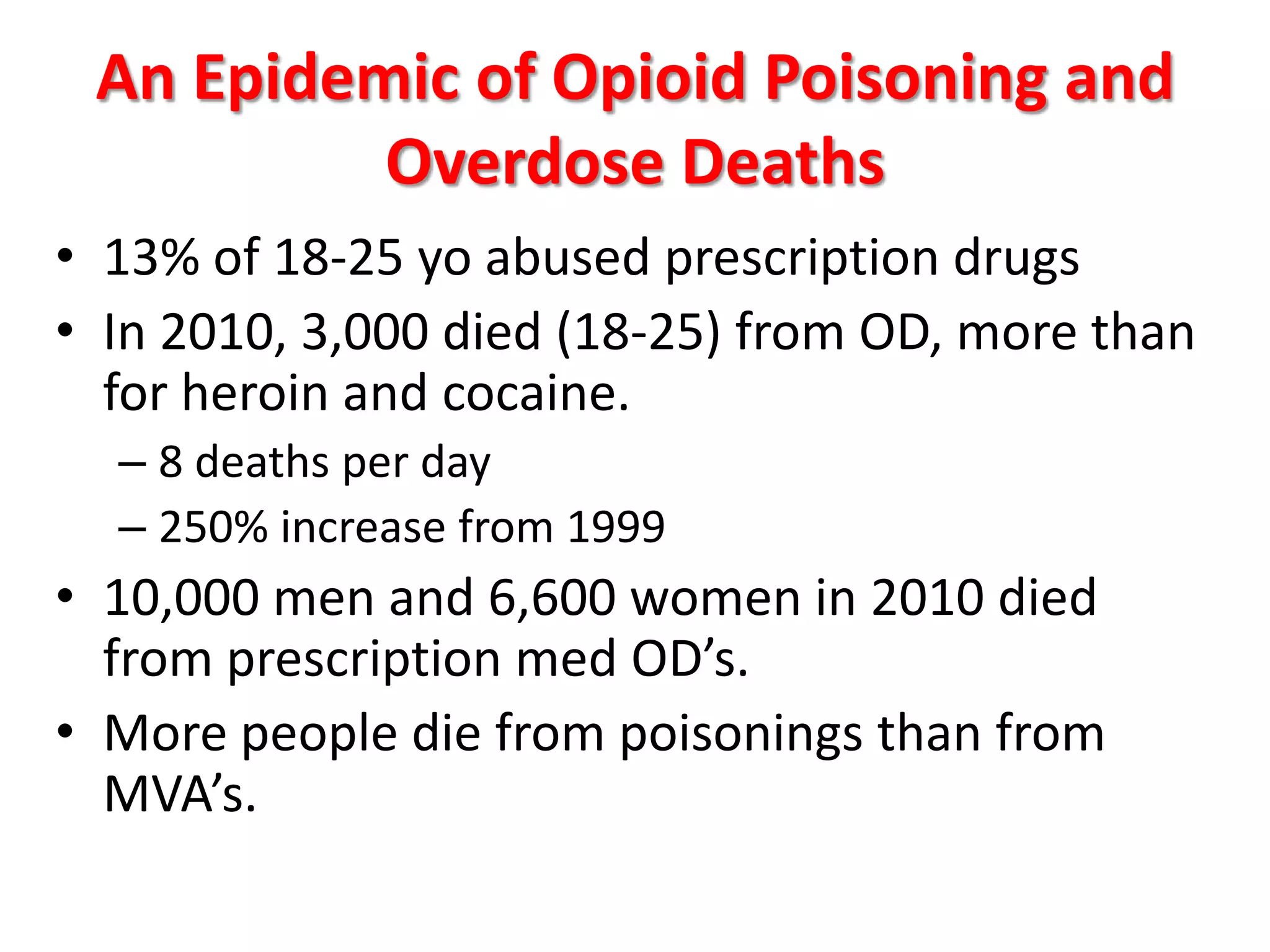
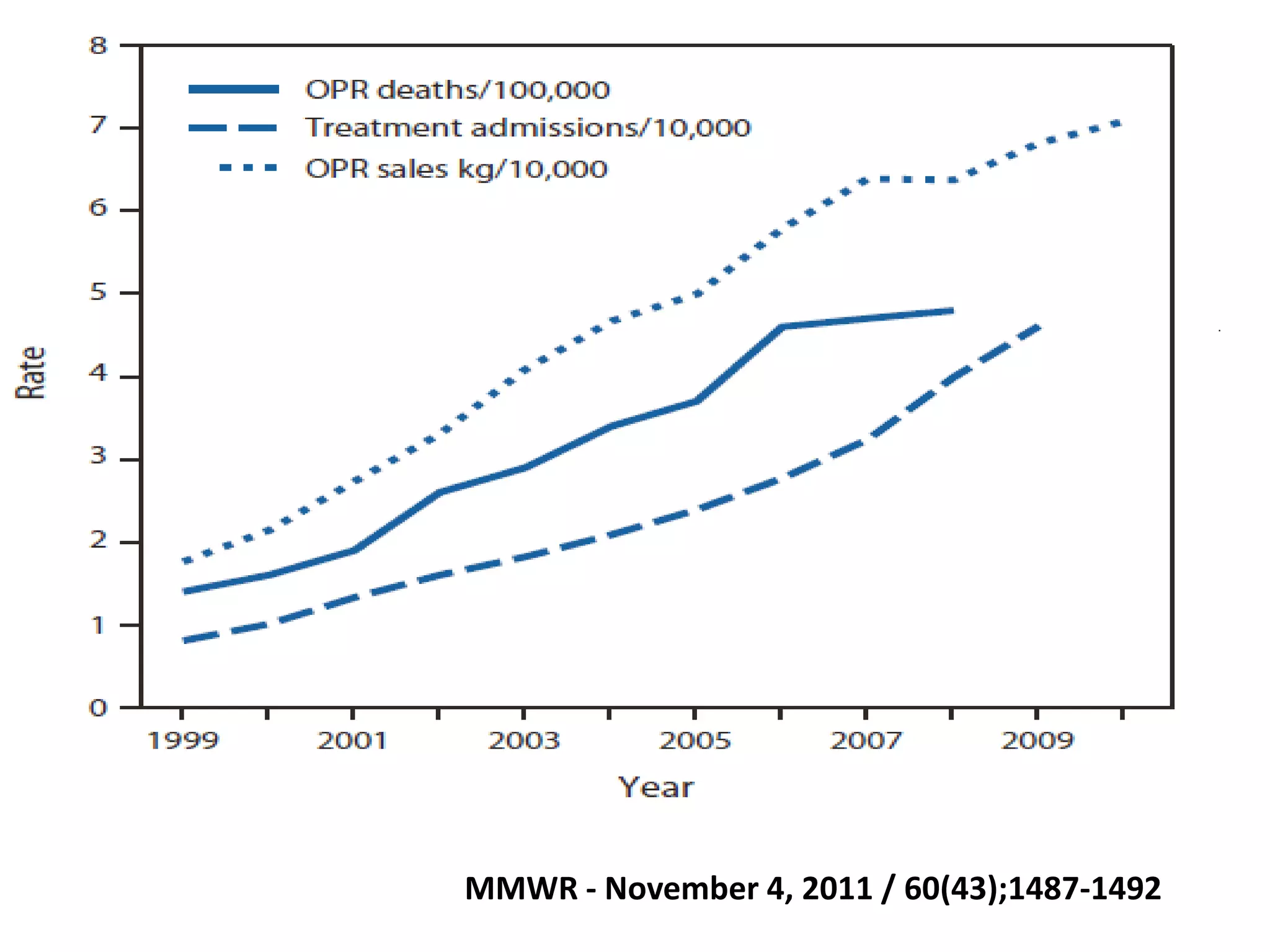
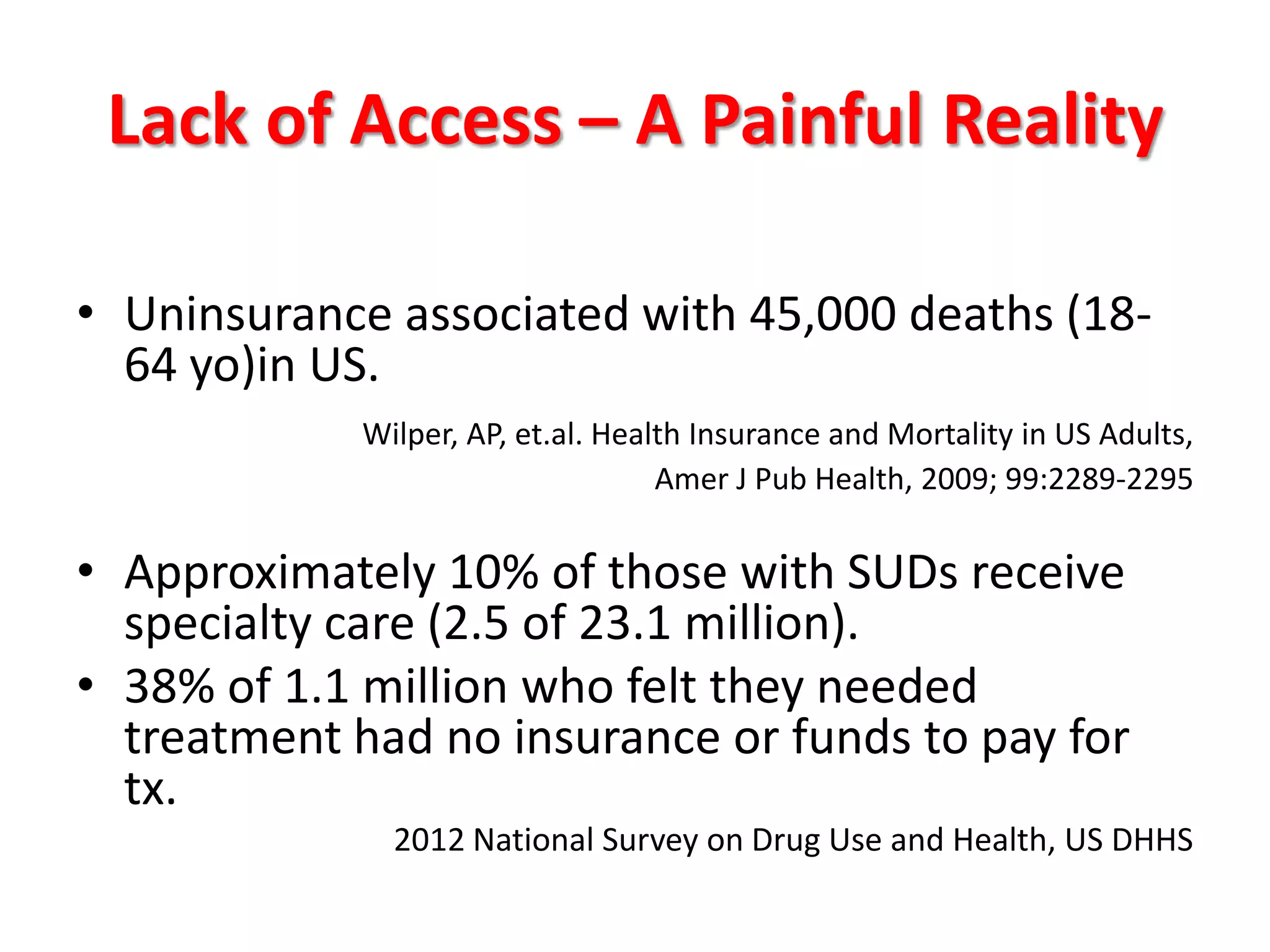
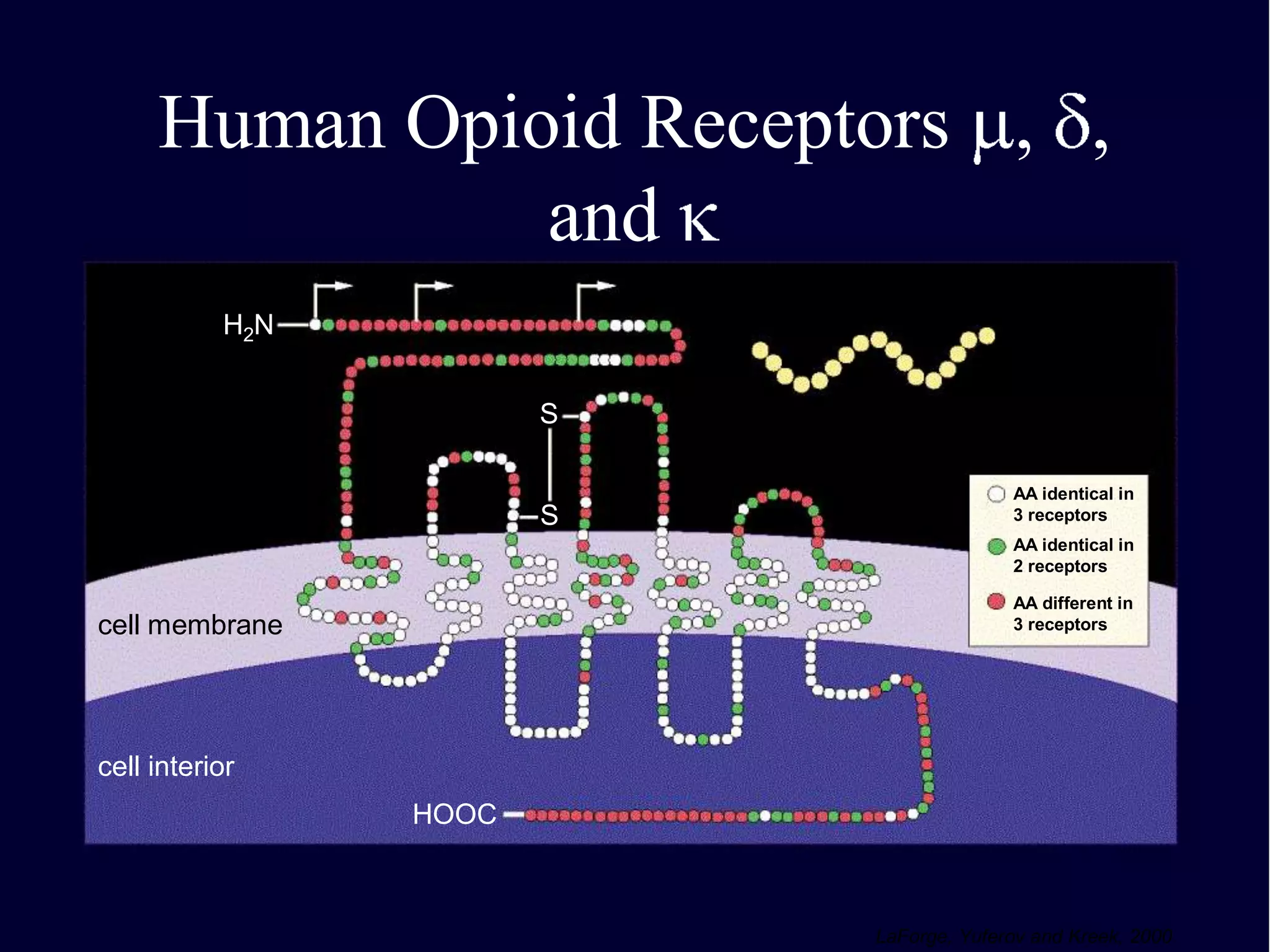
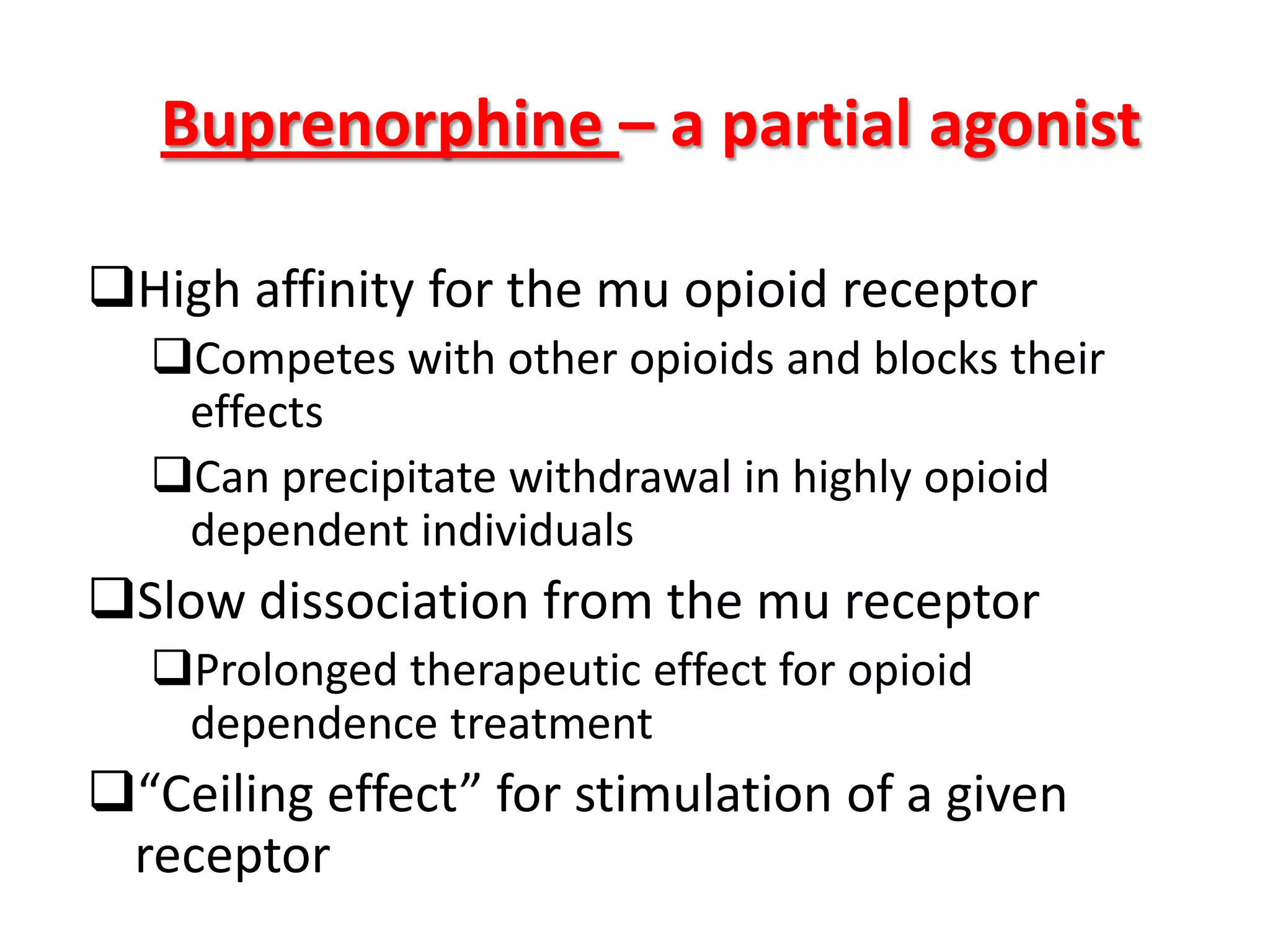
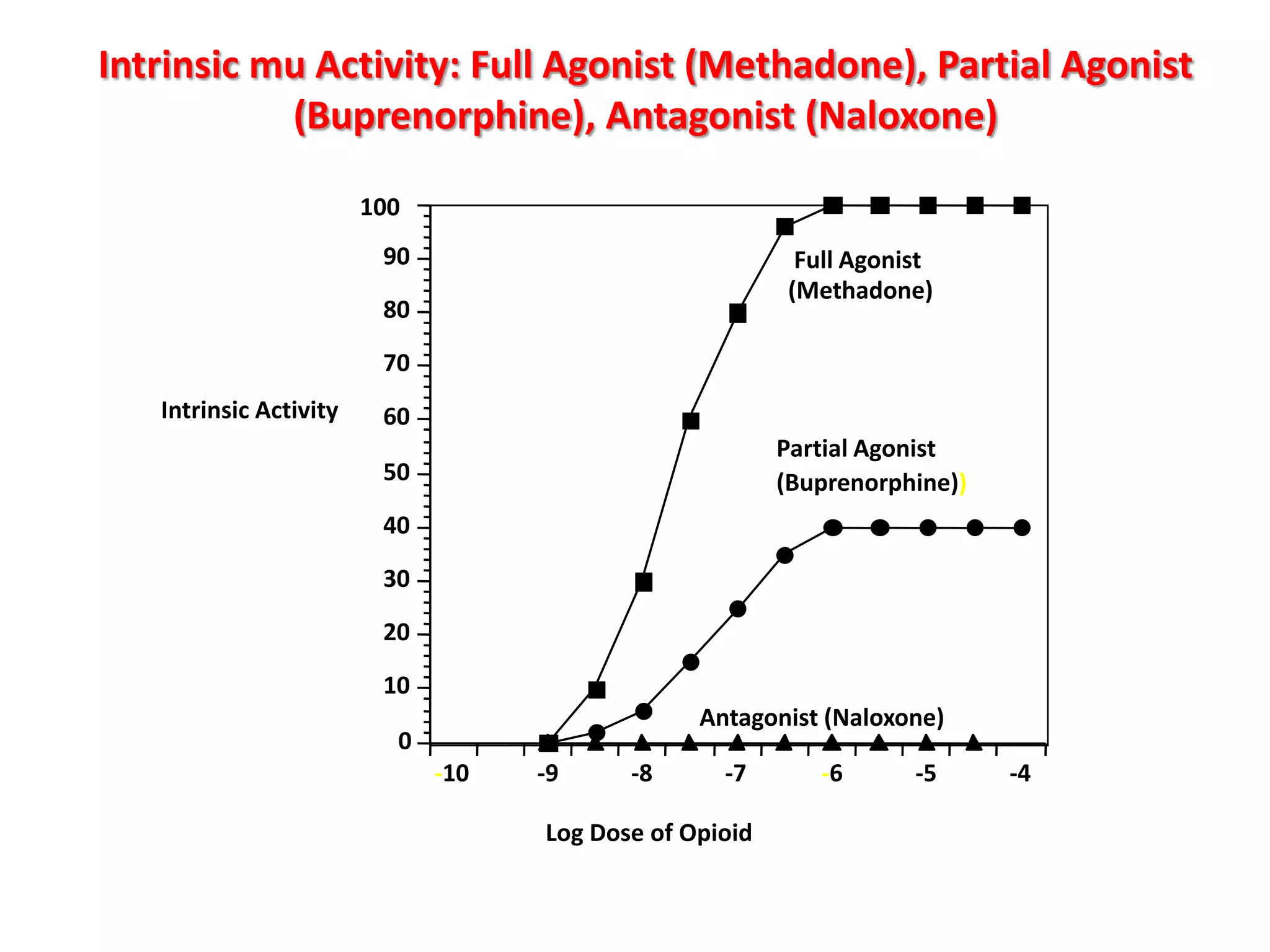
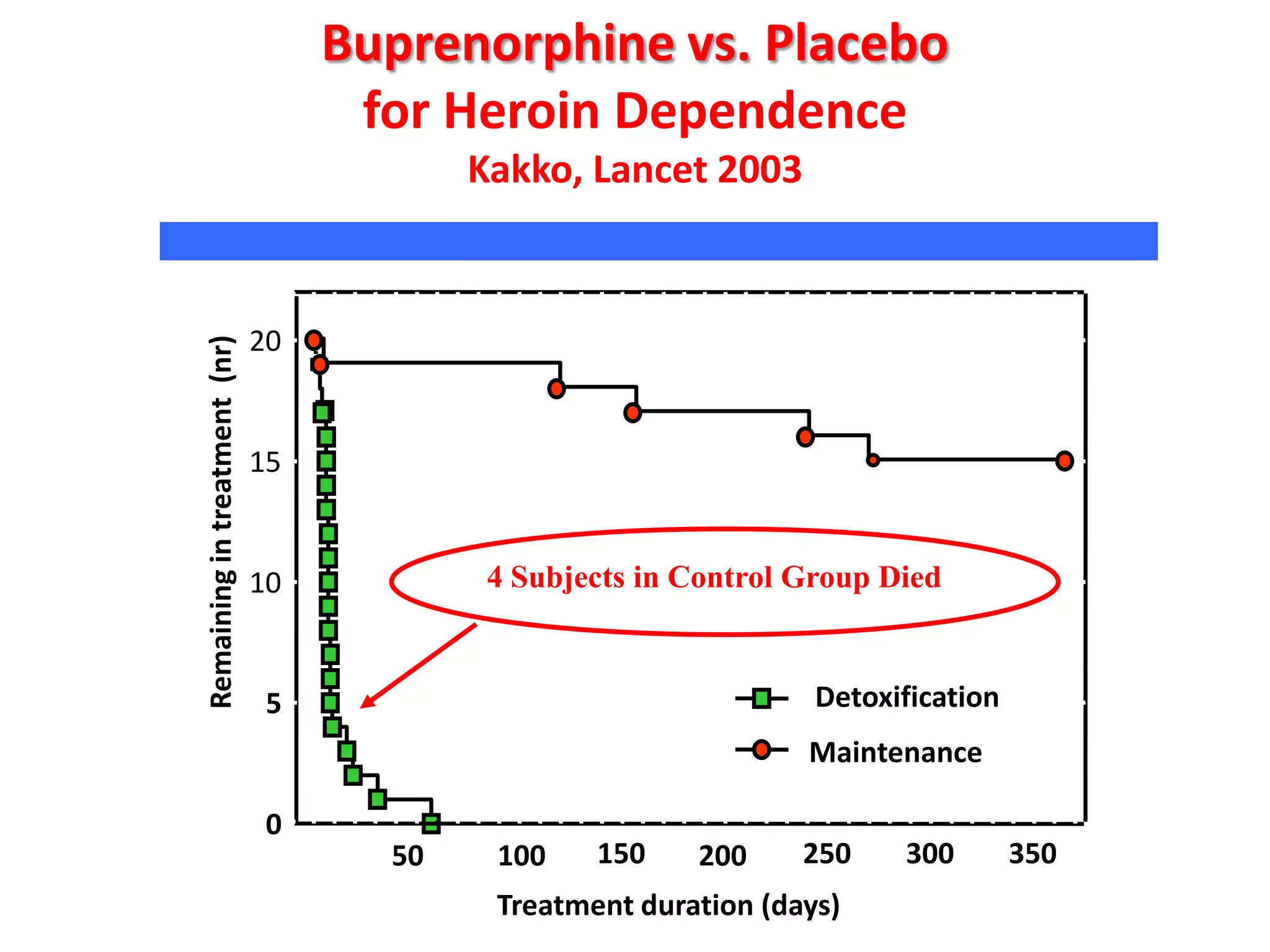
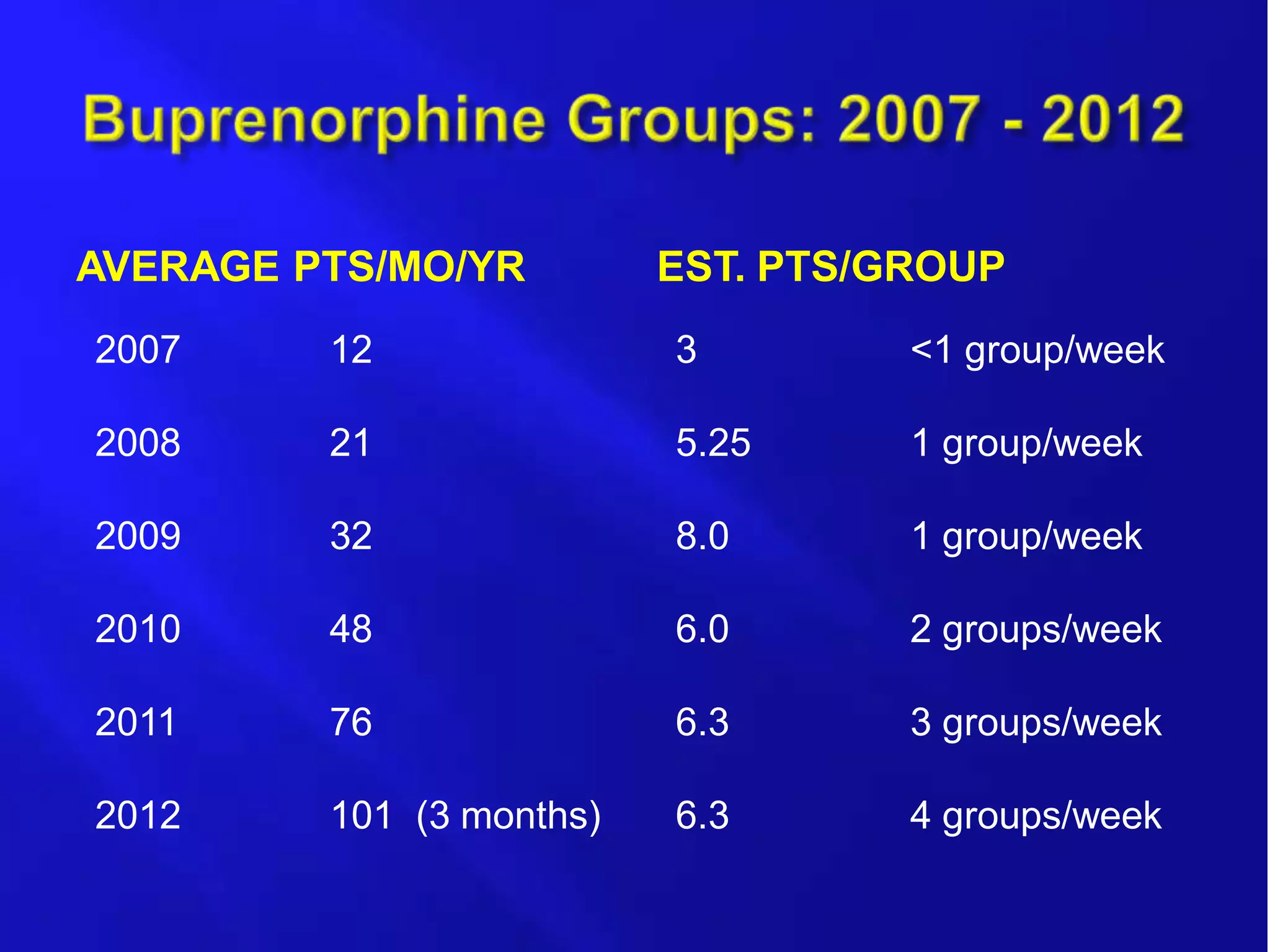
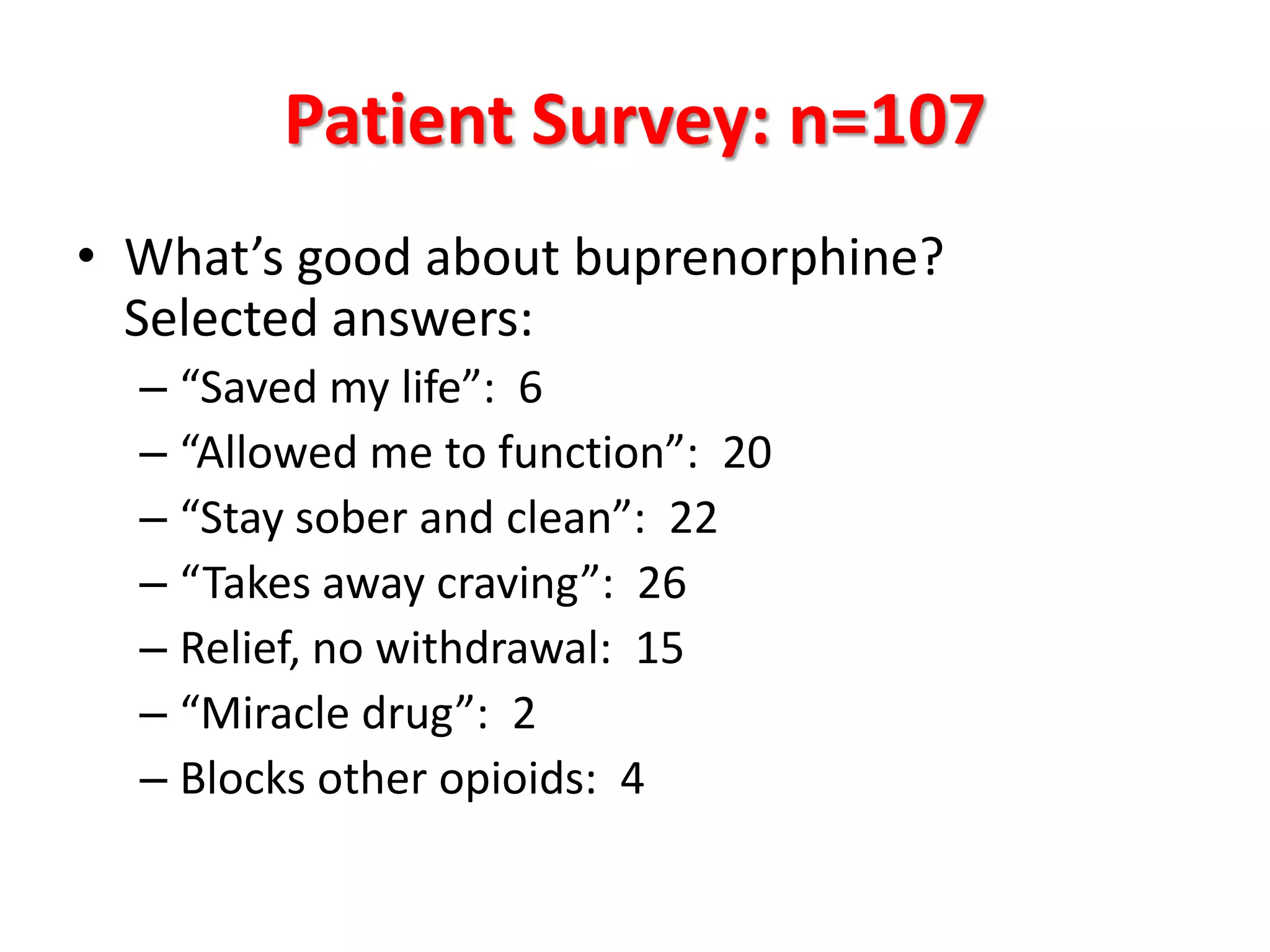
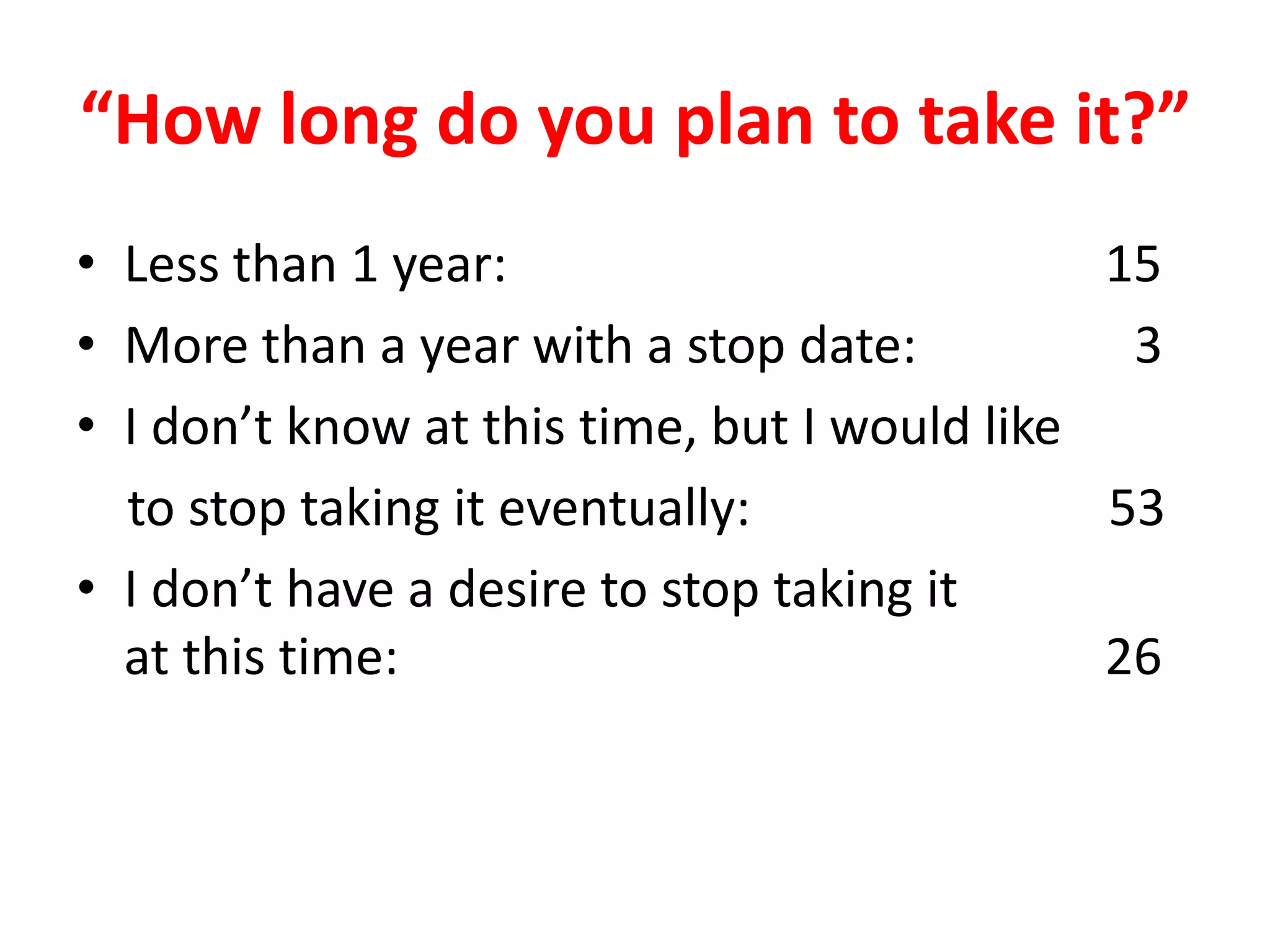
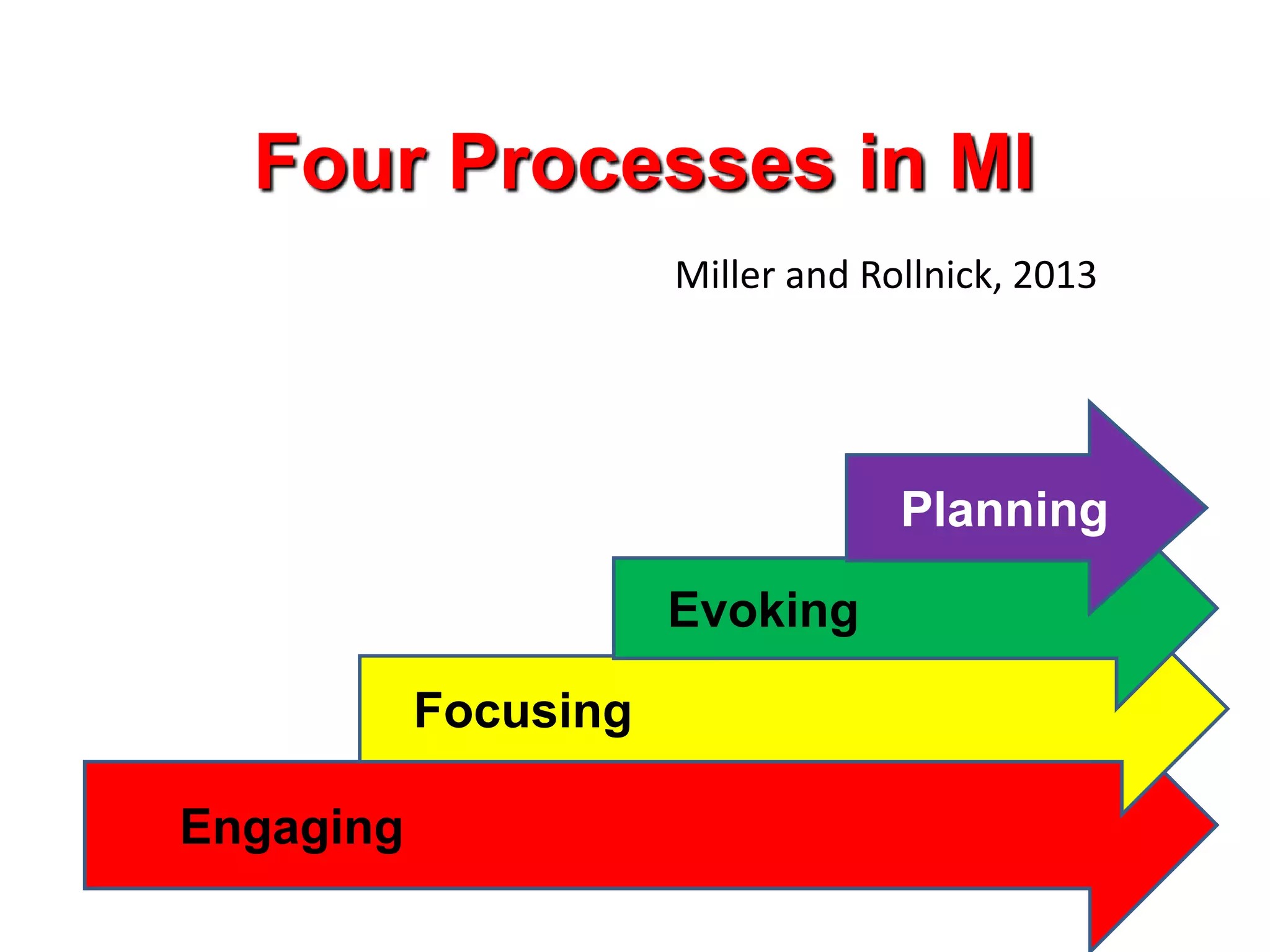
This document discusses opioid abuse and how innovation in treatment can save lives. It focuses on buprenorphine treatment for opioid addiction. Buprenorphine is a partial opioid agonist that works by blocking other opioids while reducing withdrawal symptoms and cravings. Studies show buprenorphine treatment keeps more patients in treatment programs compared to placebo. The author's clinic has successfully treated over 100 patients through buprenorphine group visits combined with counseling and motivational interviewing techniques. Patients report buprenorphine saves lives and allows them to function while remaining sober. The document concludes buprenorphine access and substance use treatment saves lives.