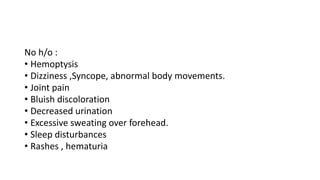
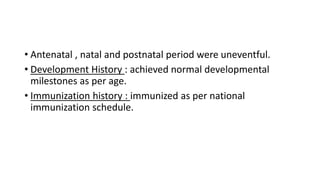
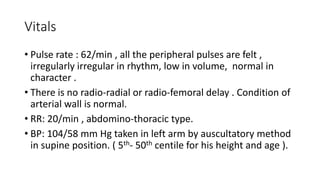
A 14-year-old boy presented with difficulty breathing, facial swelling, swelling of both feet, and chest pain for two days. He had a history of a similar episode 8 months prior where he was diagnosed with a heart condition. On examination, he had an irregularly irregular pulse, low blood pressure, visible apex beat, and grade V pansystolic murmurs in the mitral, tricuspid, and pulmonary areas, suggestive of chronic rheumatic heart disease with mitral regurgitation and left ventricular hypertrophy.