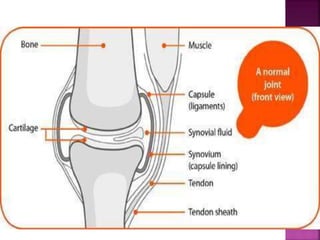
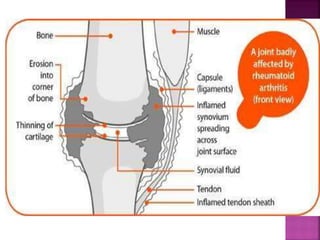
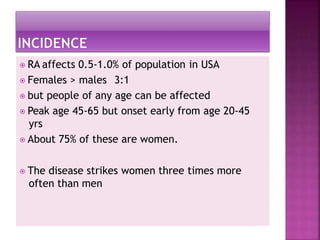
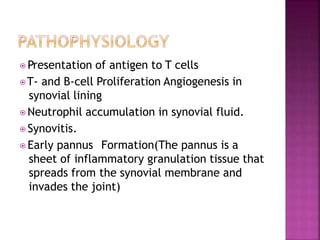
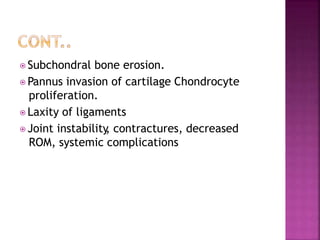
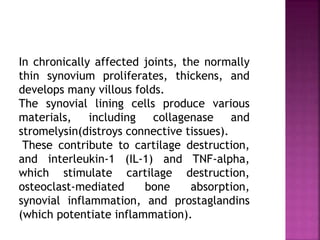
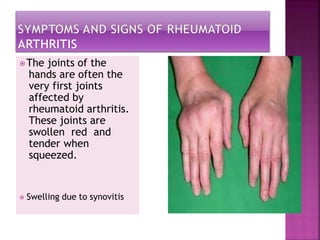
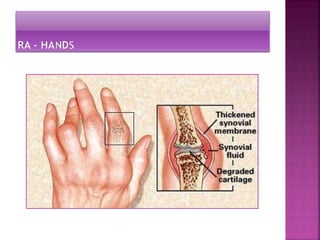
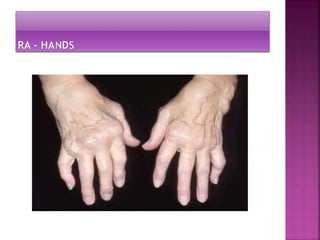
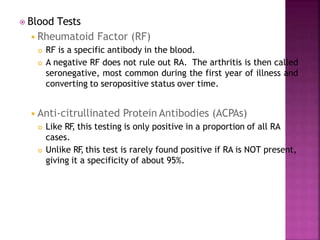
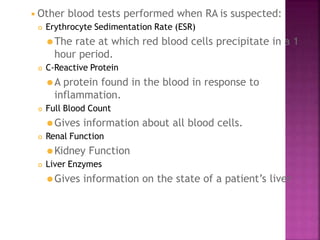
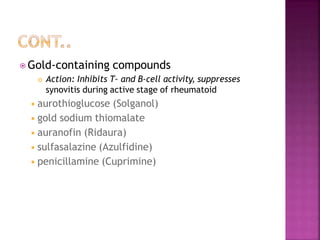
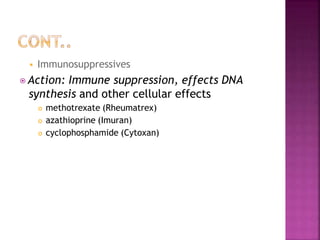
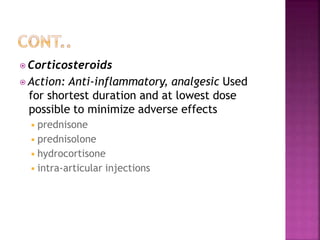
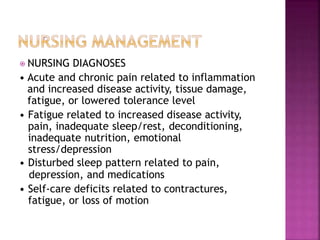
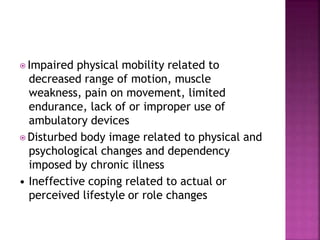
Rheumatoid arthritis is an autoimmune disorder where the immune system attacks the synovial membrane lining the joints, causing inflammation. It commonly first affects small joints in the hands and can lead to joint deformity, damage, and disability over time. Treatments include medications like NSAIDs, DMARDs, steroids and biologics, as well as exercise and surgery. Ankylosing spondylitis is a related inflammatory arthritis that primarily affects the spine, causing fusion of vertebrae and a stooped posture. It has genetic and environmental risk factors and is treated with exercise, NSAIDs, and biologics. Graft-versus-host disease occurs when donor immune cells in a bone marrow transplant attack