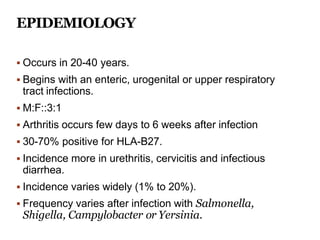
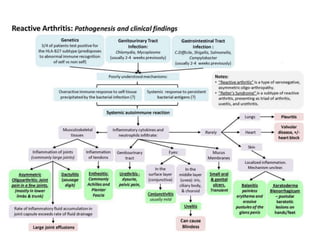
The patient presented with acute arthritis in both knees after experiencing diarrhea for 10 days previously. He also had red eyes for a week. Examination found joint tenderness, redness and effusions in both knees. Tests found elevated ESR and CRP but no crystals or organisms in synovial fluid. He was HLA-B27 positive. He was diagnosed with reactive arthritis triggered by a previous enteric infection, as evidenced by his diarrhea, and was started on indomethacin with improvement of symptoms.
![ Kim PS, Klausmeier TL, Orr DP. Reactive arthritis: a review. Journal of Adolescent Health. 2009
Apr 1;44(4):309-15.
Cheeti A, Chakraborty RK, Ramphul K. Reactive Arthritis (Reiter Syndrome). InStatPearls
[Internet] 2020 Mar 13. StatPearls Publishing.
Stavropoulos PG, Soura E, Kanelleas A, Katsambas A, Antoniou C. Reactive arthritis. Journal of
the European Academy of Dermatology and Venereology. 2015 Mar;29(3):415-24.
García-Kutzbach A, Chacón-Súchite J, García-Ferrer H, Iraheta I. Reactive arthritis: update
2018. Clinical Rheumatology. 2018 Apr 1;37(4):869-74.
Colmegna I, Cuchacovich R, Espinoza LR. HLA-B27-associated reactive arthritis: pathogenetic
and clinical considerations. Clinical microbiology reviews. 2004 Apr 1;17(2):348-69.
Carter JD. Treating reactive arthritis: insights for the clinician. Therapeutic advances in
musculoskeletal disease. 2010 Feb;2(1):45-54.
Mukherjee S, Kar M. Reactive arthritis: current perspectives. J Ind Acad Clin Med. 2000
Oct;1:233-8.
Selmi C, Gershwin ME. Diagnosis and classification of reactive arthritis. Autoimmunity reviews.
2014 Apr 1;13(4-5):546-9.
HARRISON B, SILMAN A, SYMMONS D. Diagnostic evaluation of classification criteria for RA
and reactive arthritis. Annals of the Rheumatic Diseases. 2000 May 1;59(5):397-8.](https://image.slidesharecdn.com/reactivearthritis-201029161901-240329111957-87d442ee/85/reactivearthritis-2bbbbbbb01029161901-pptx-29-320.jpg)
