This document provides an overview of how to approach connective tissue disorders. It discusses:
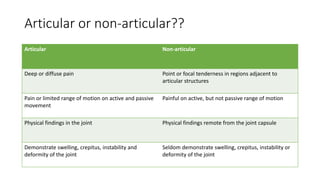
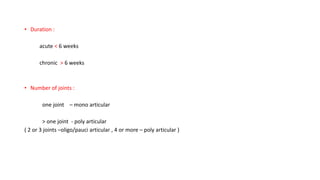
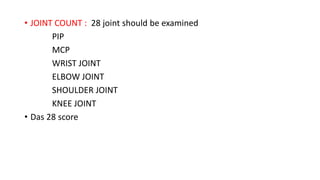
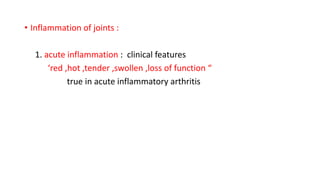
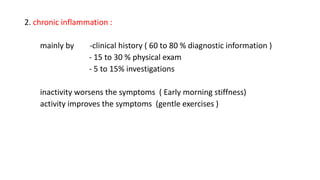
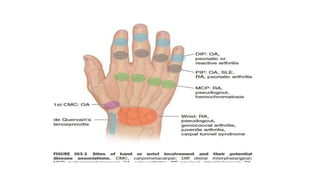
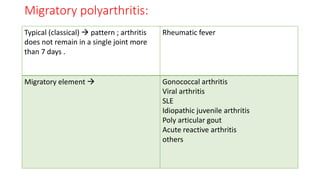
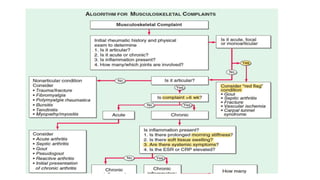
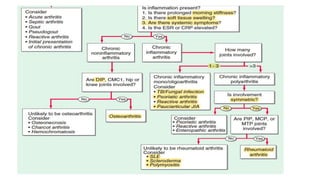
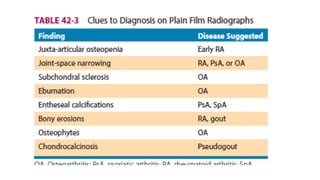
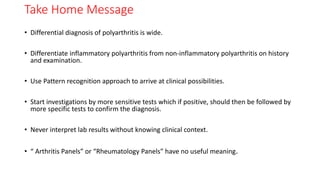
1. The importance of taking a thorough history and physical exam to determine if the condition is articular or non-articular, acute or chronic, and which joints are involved.
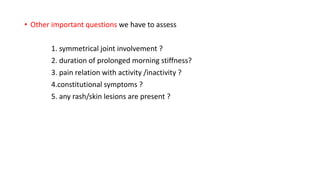
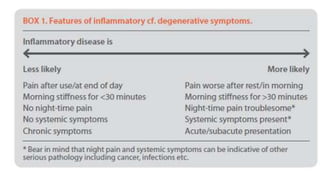
2. Key questions to ask patients around joint involvement, morning stiffness, pain with activity, and constitutional symptoms.
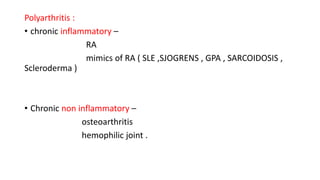
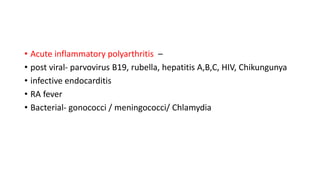
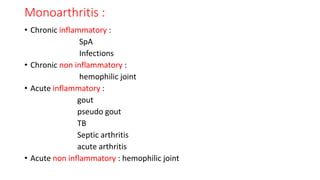
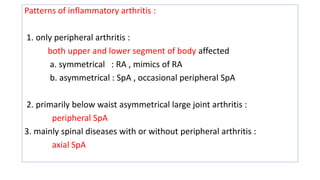
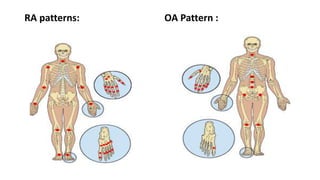
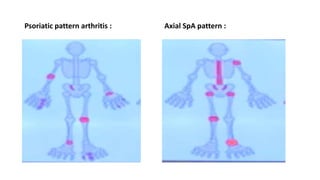
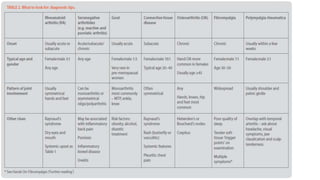
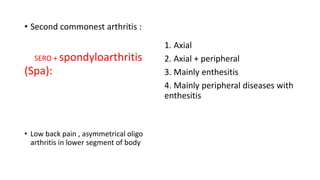
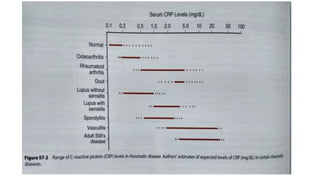
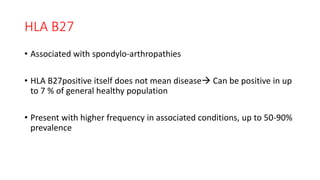
3. Common patterns seen in different diseases like rheumatoid arthritis, spondyloarthropathies, and osteoarthritis.
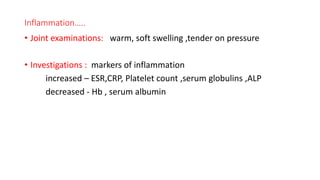
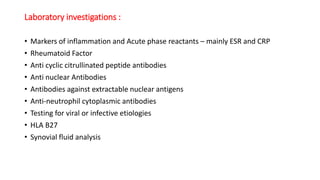
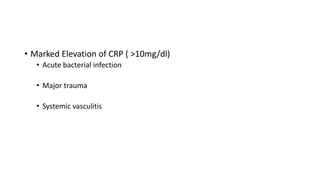
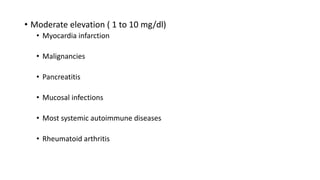
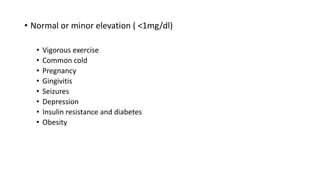
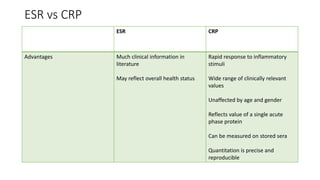
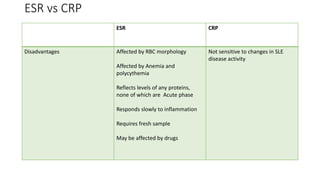
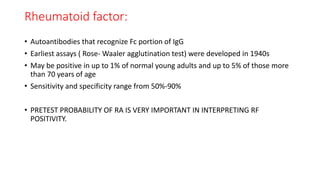
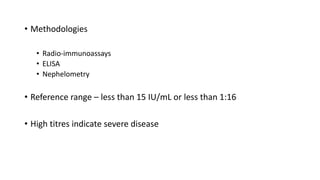
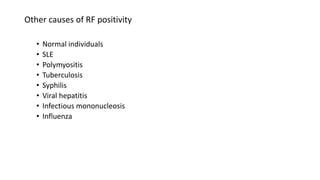
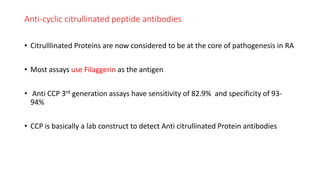
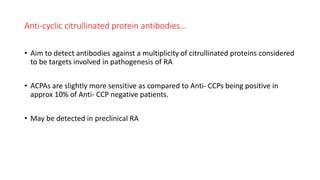
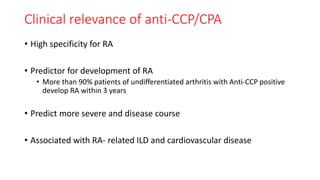
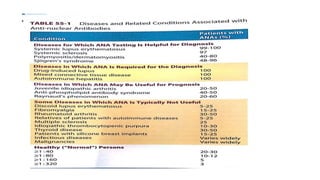
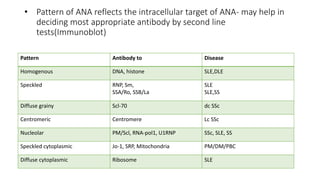
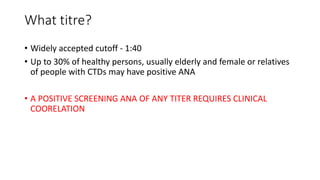
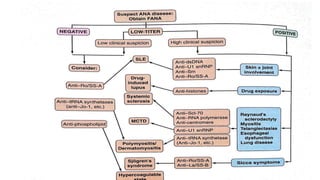
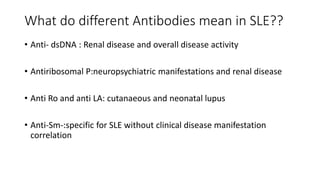
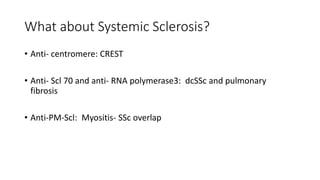
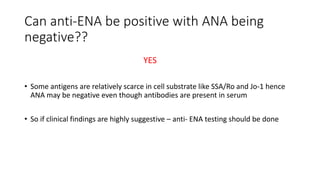
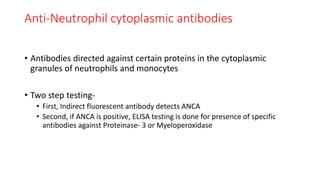
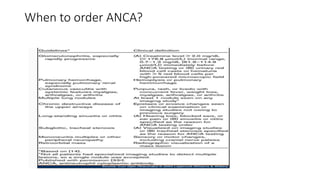
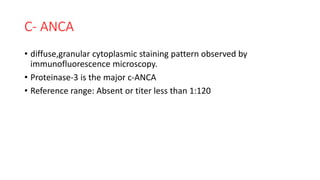
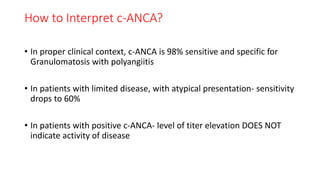
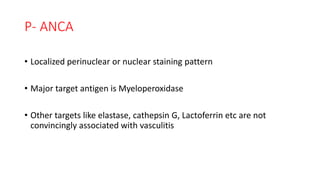
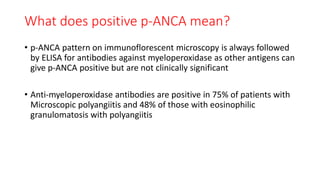
4. The role of various laboratory tests like ESR, CRP, rheumatoid factor, anti-CCP, ANA, and ANCA in evaluating patients and supporting diagnoses.