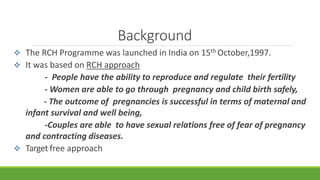
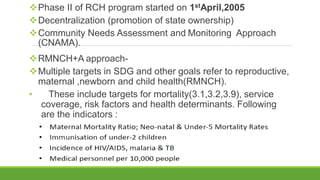
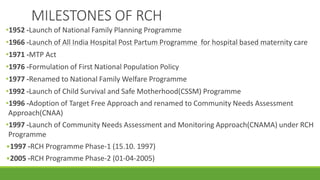
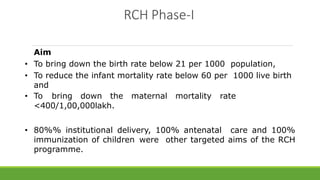
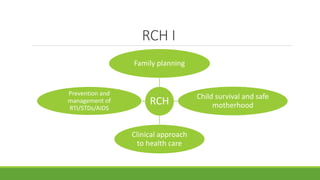
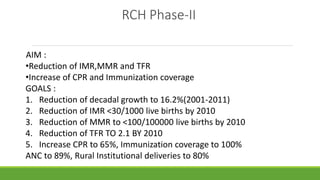
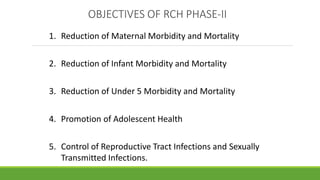
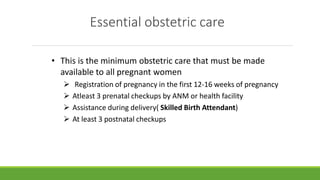
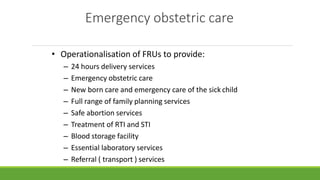
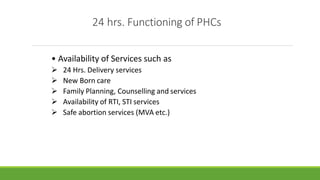
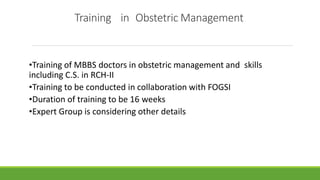
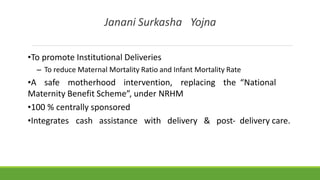
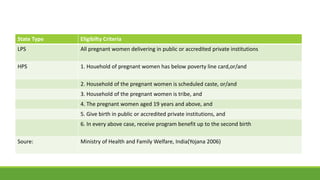
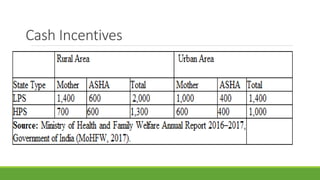
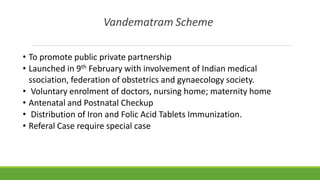
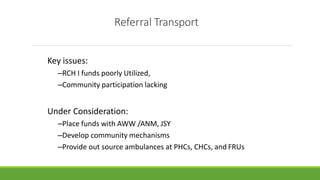
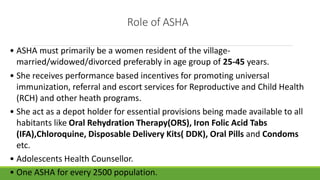
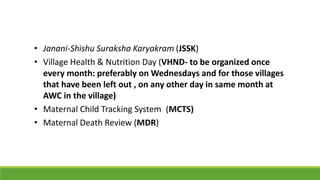
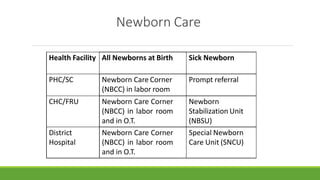
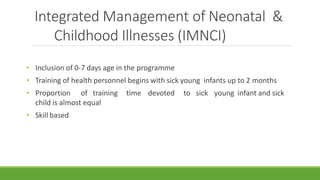
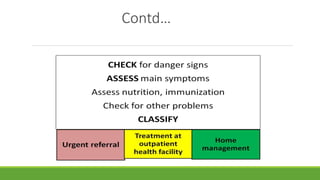
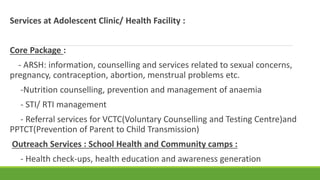
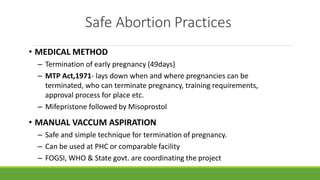
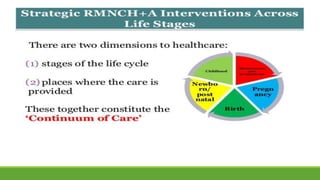
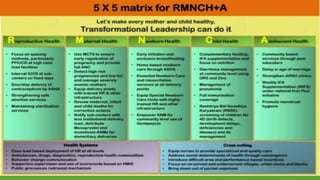
The document summarizes key aspects of India's Reproductive and Child Health (RCH) program. It discusses the phases and goals of RCH Phase I and Phase II, including targets for reducing infant mortality, maternal mortality, and total fertility rates. It describes essential components of RCH like antenatal care, skilled birth attendance, emergency obstetric care, and new initiatives under RCH II such as Janani Suraksha Yojana cash incentives for institutional deliveries. The role of ASHAs in community health and new approaches like IMNCI and RMNCH+A are also highlighted.