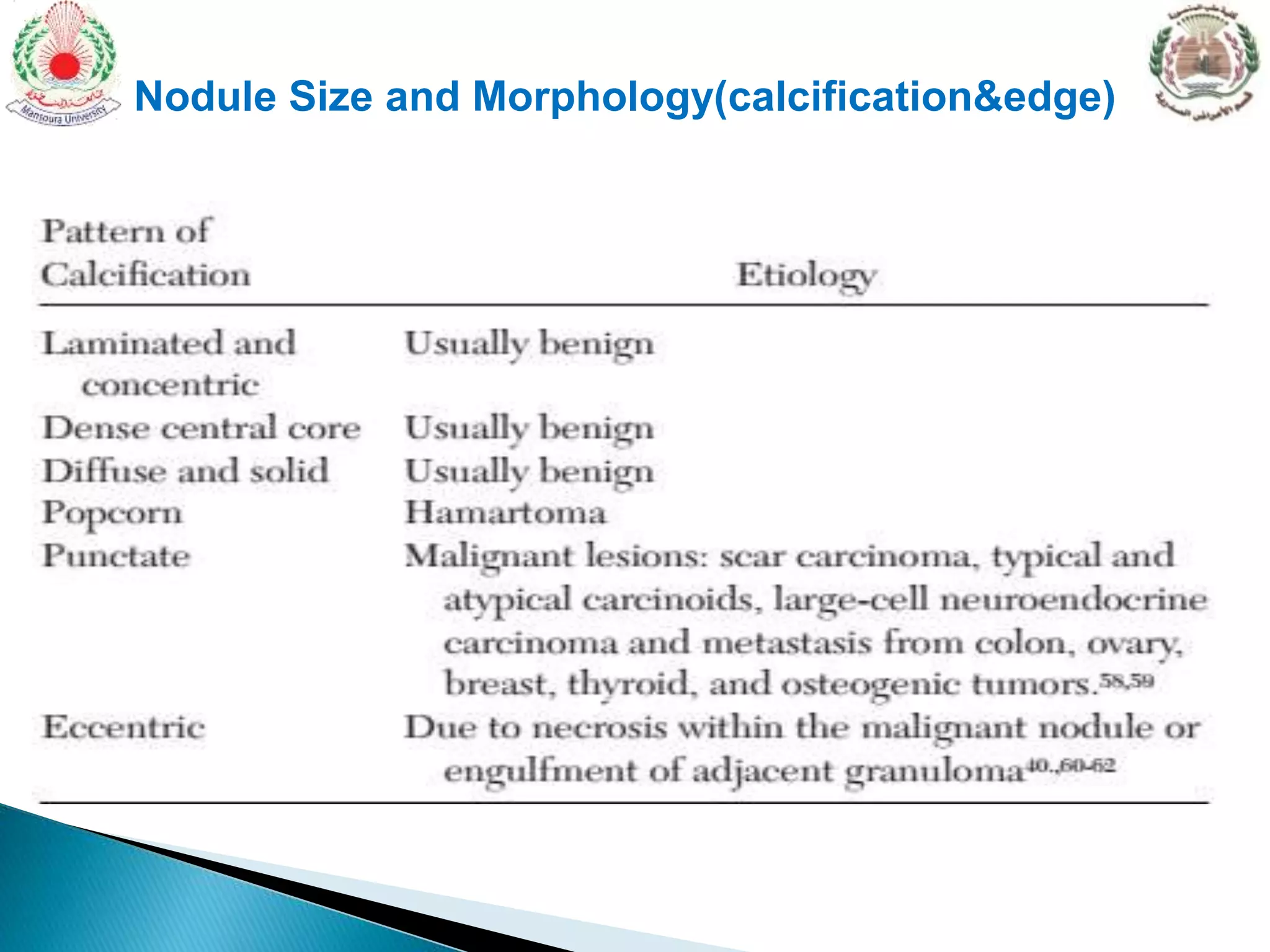
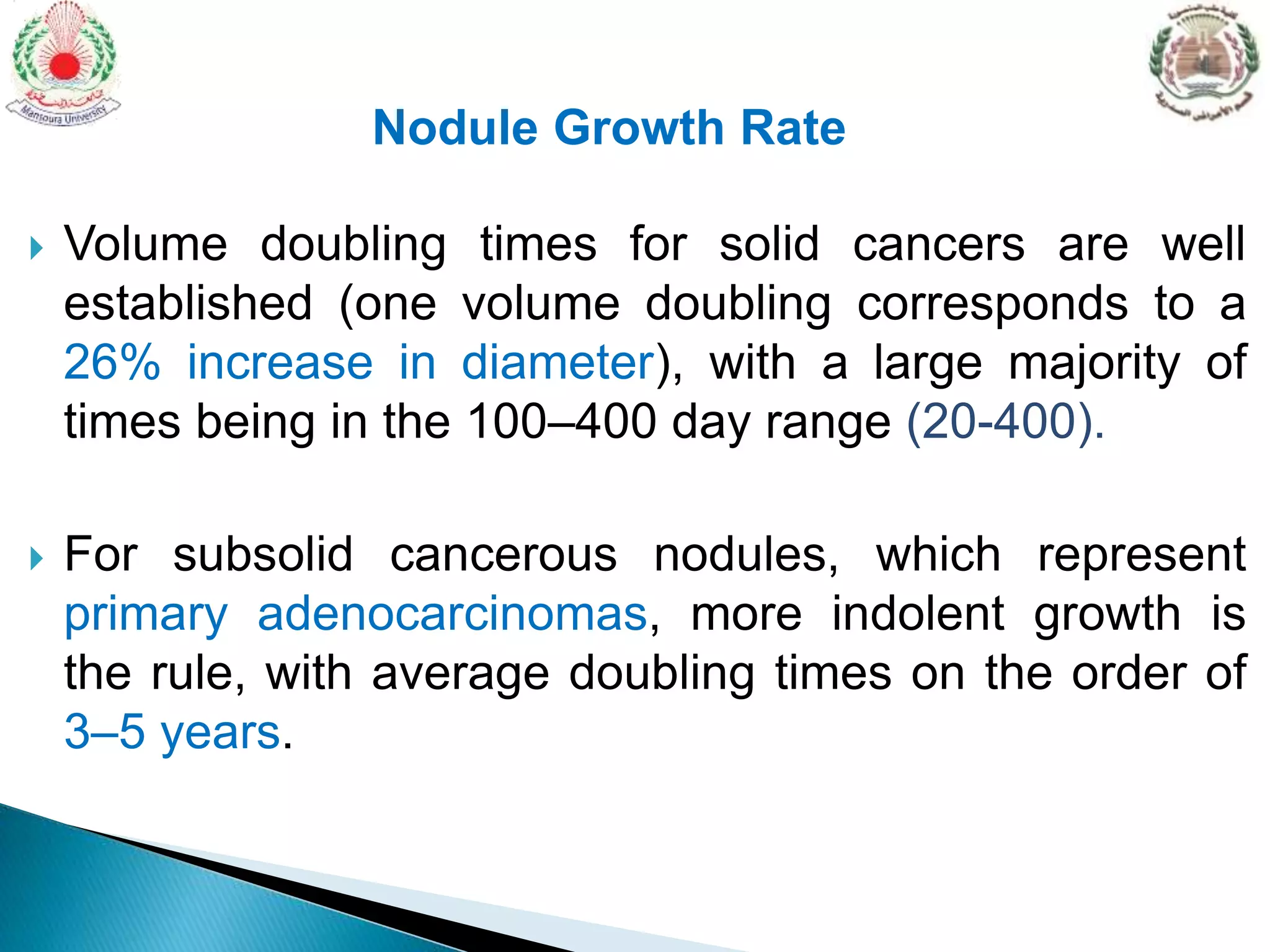
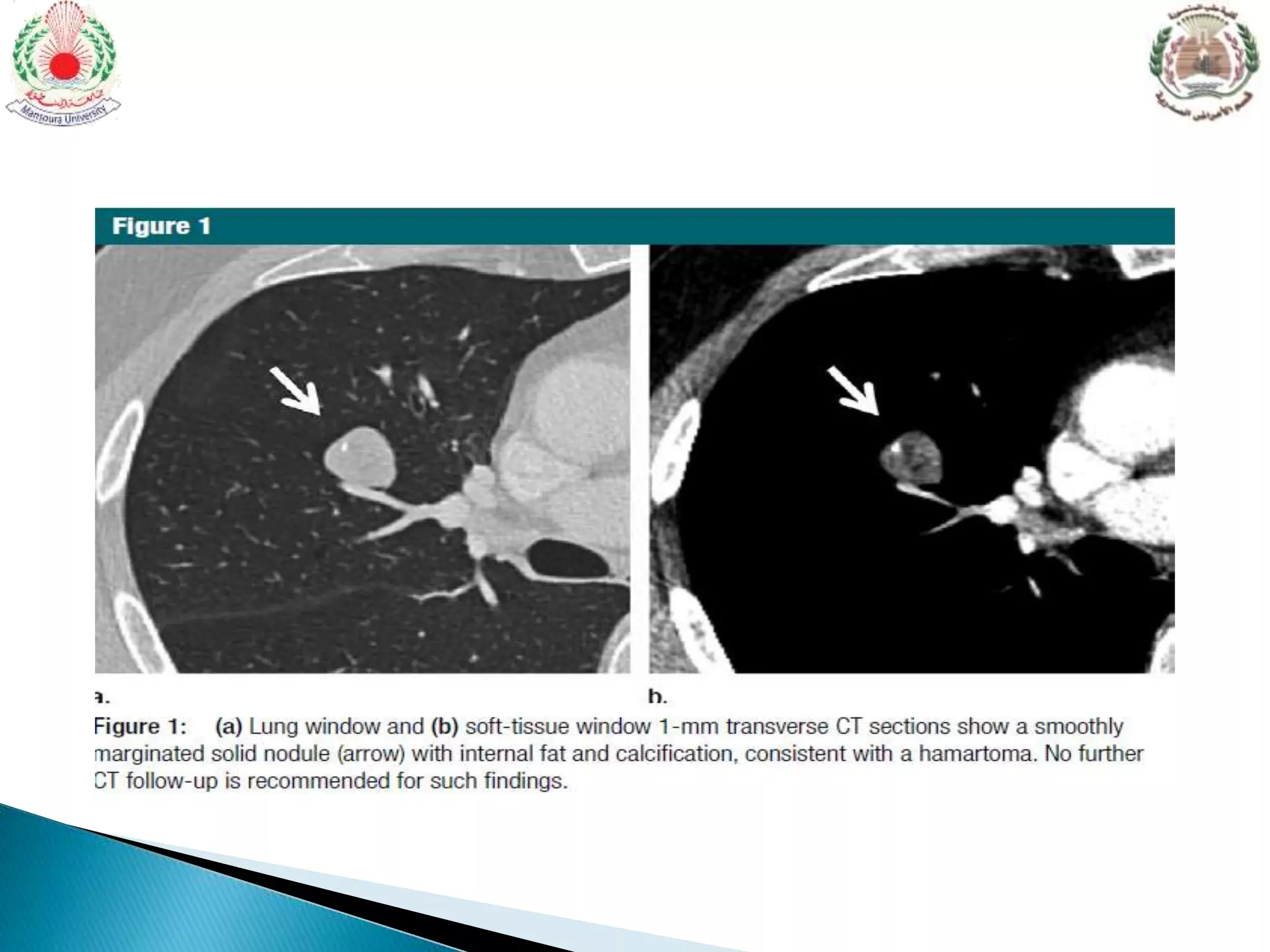
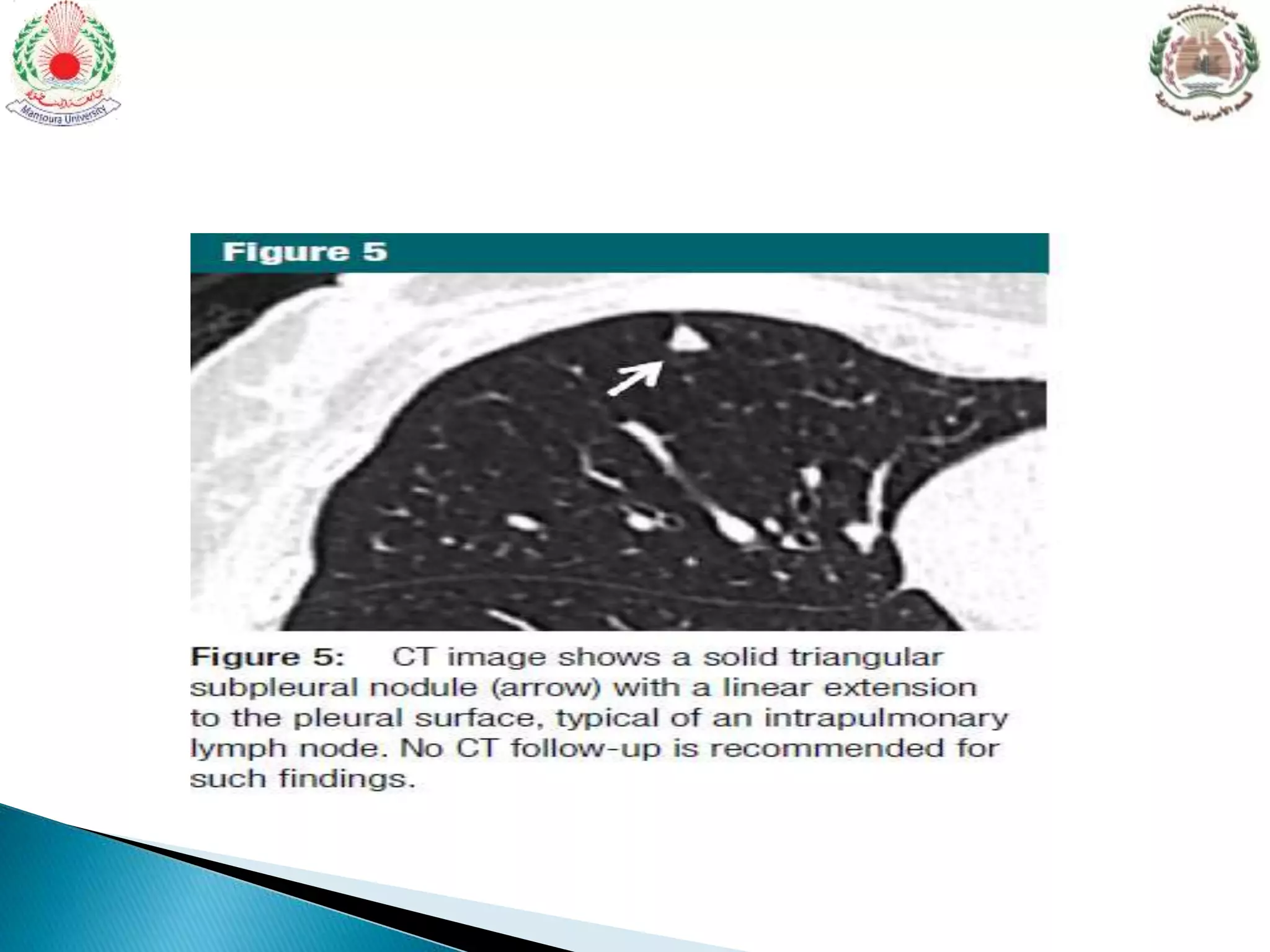
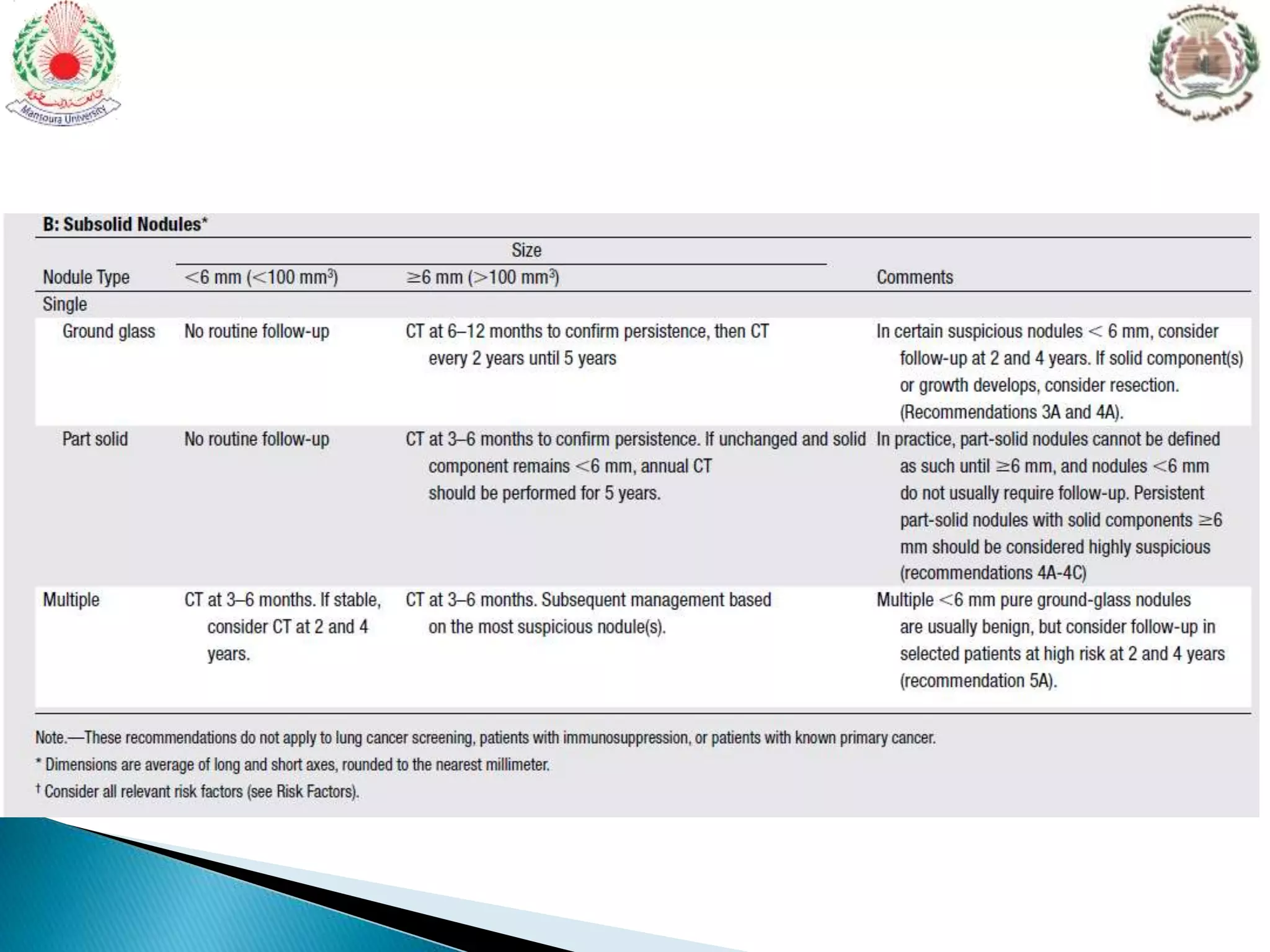
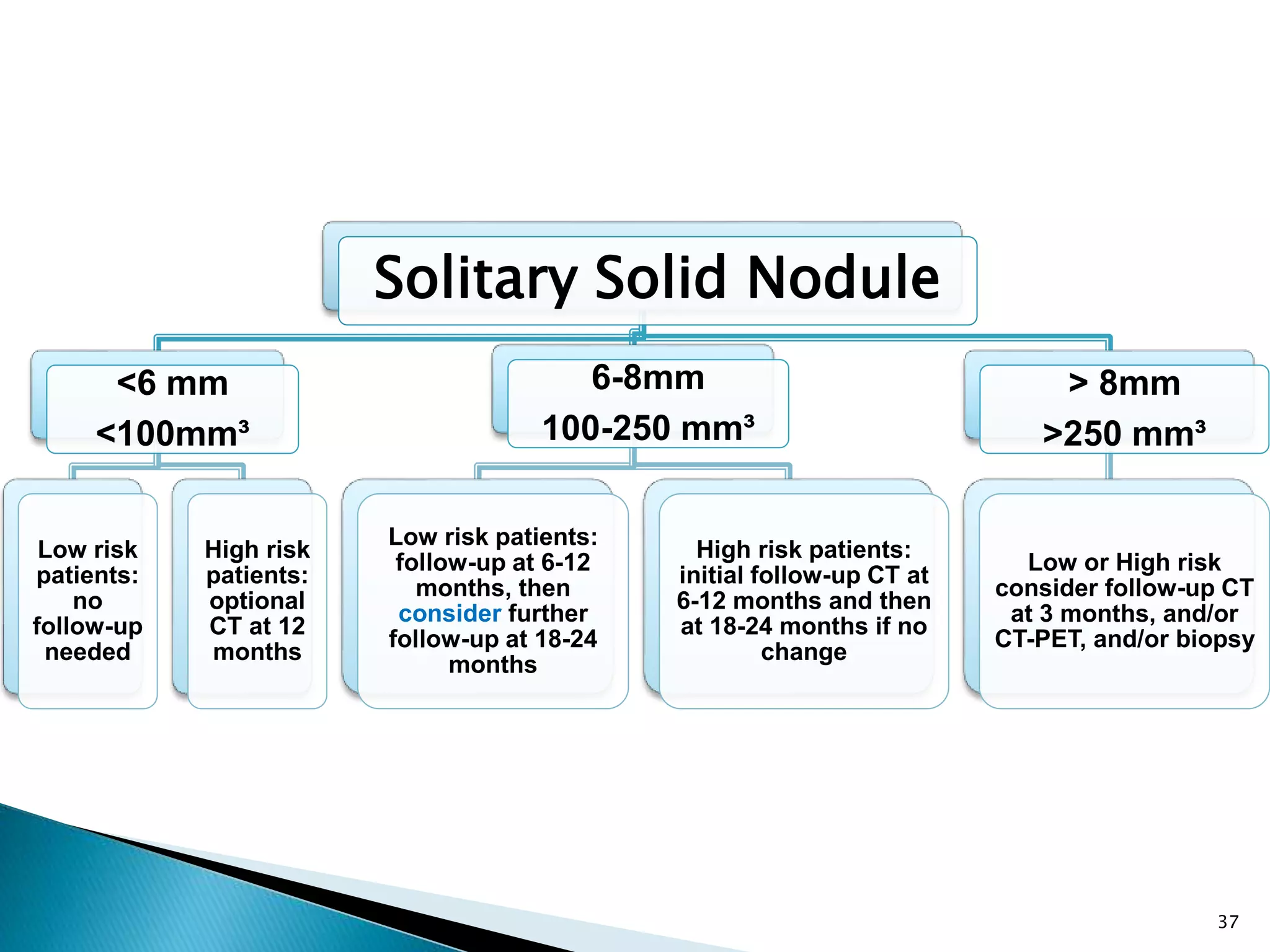
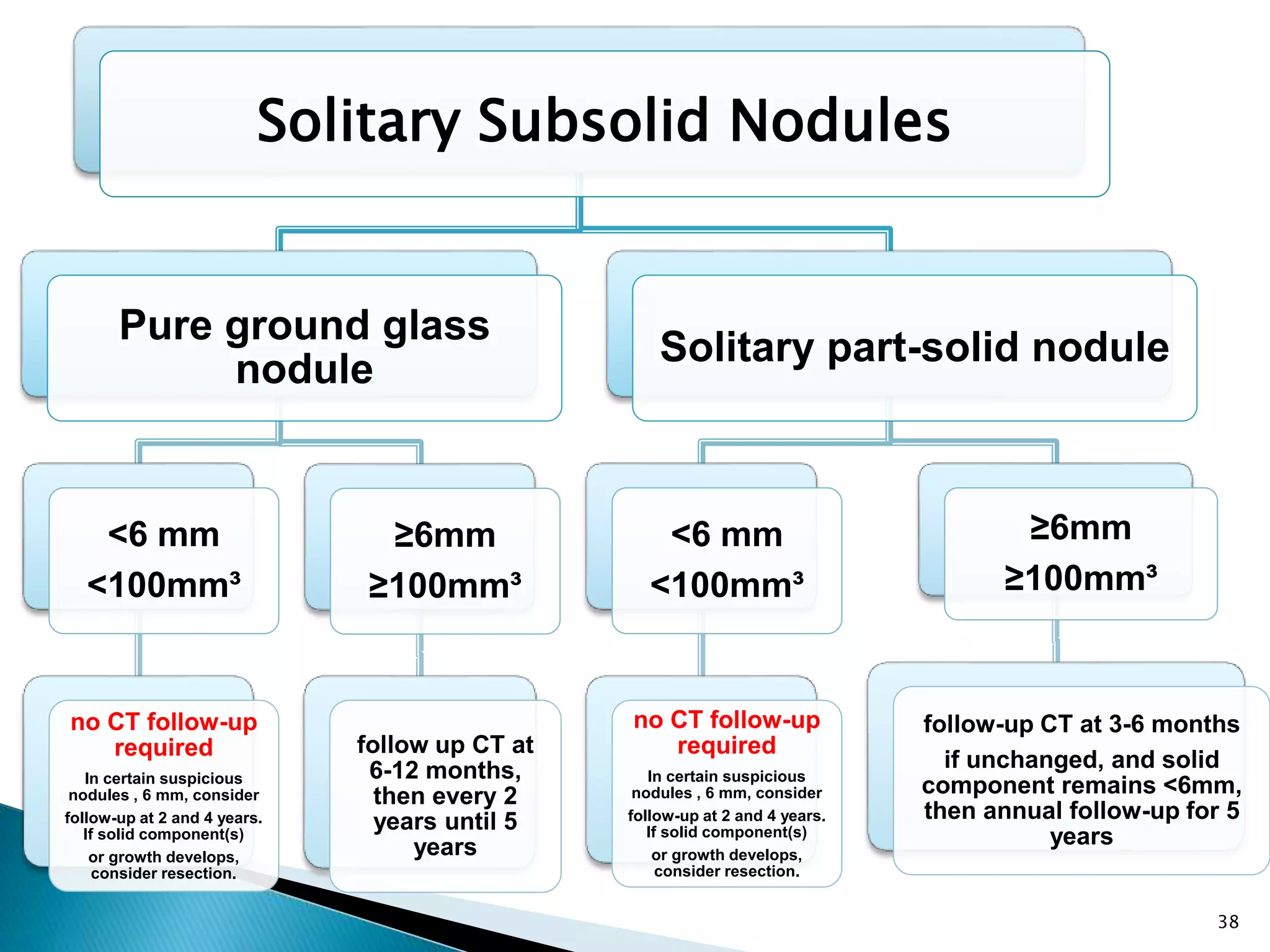
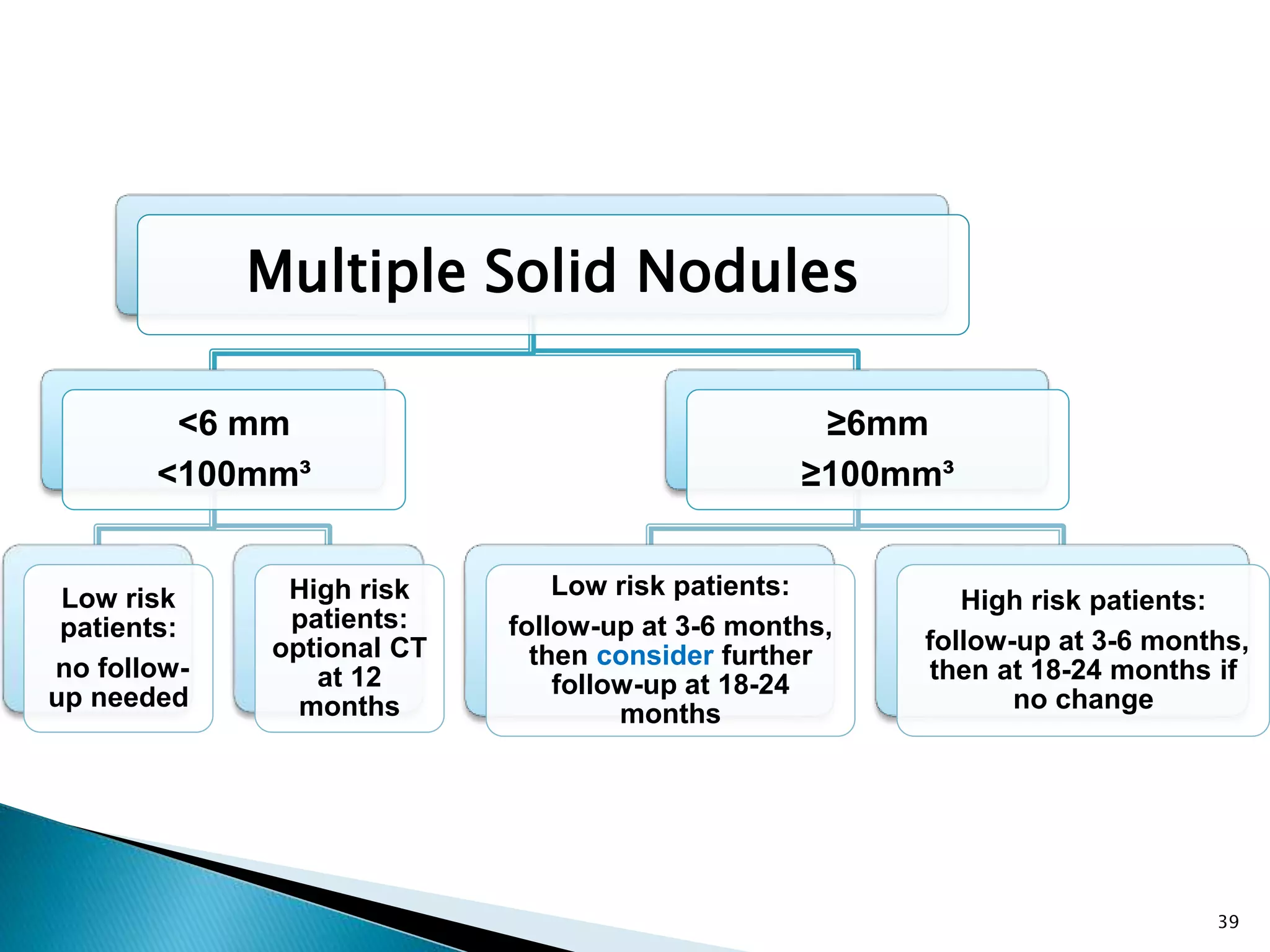
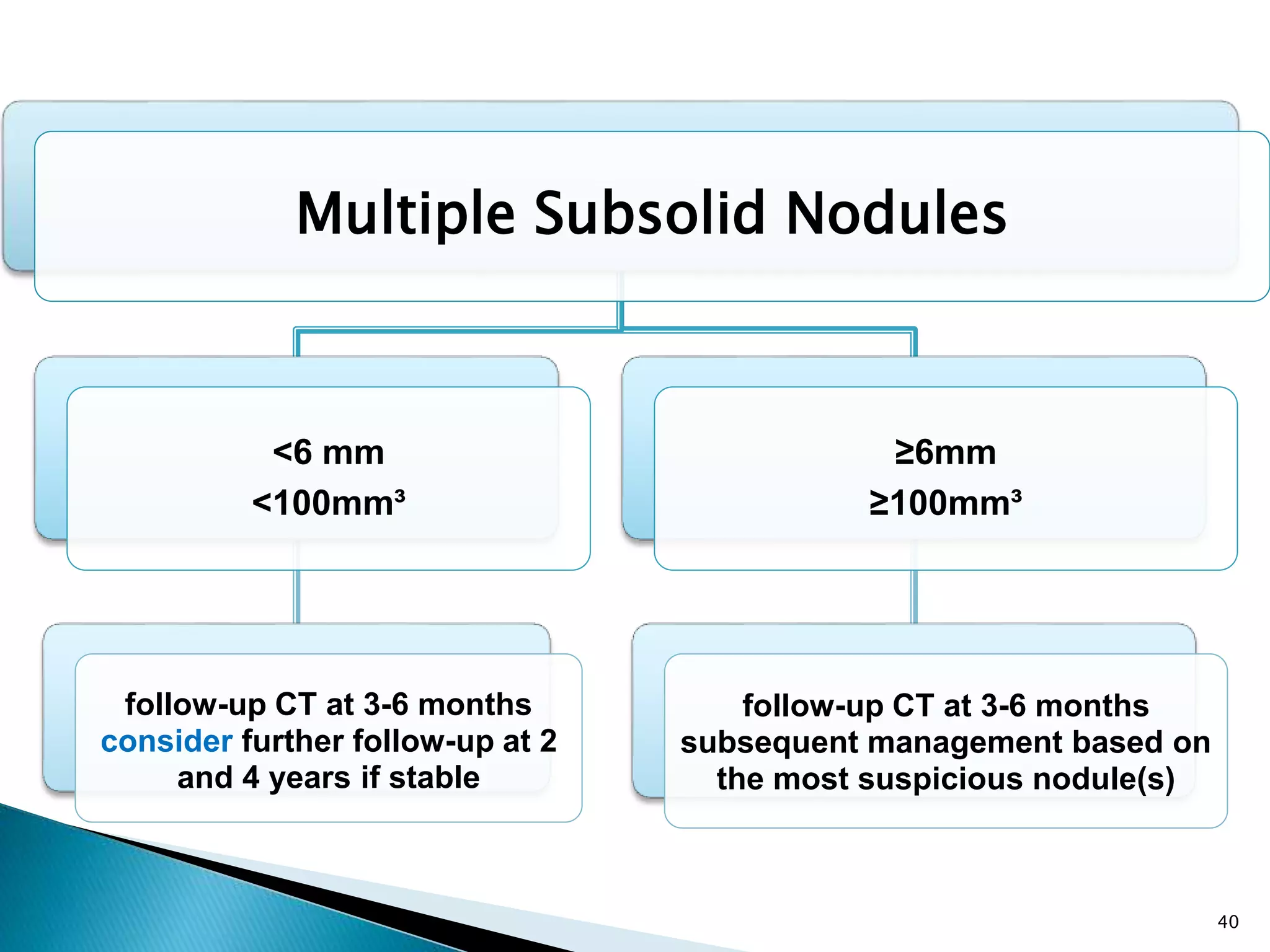
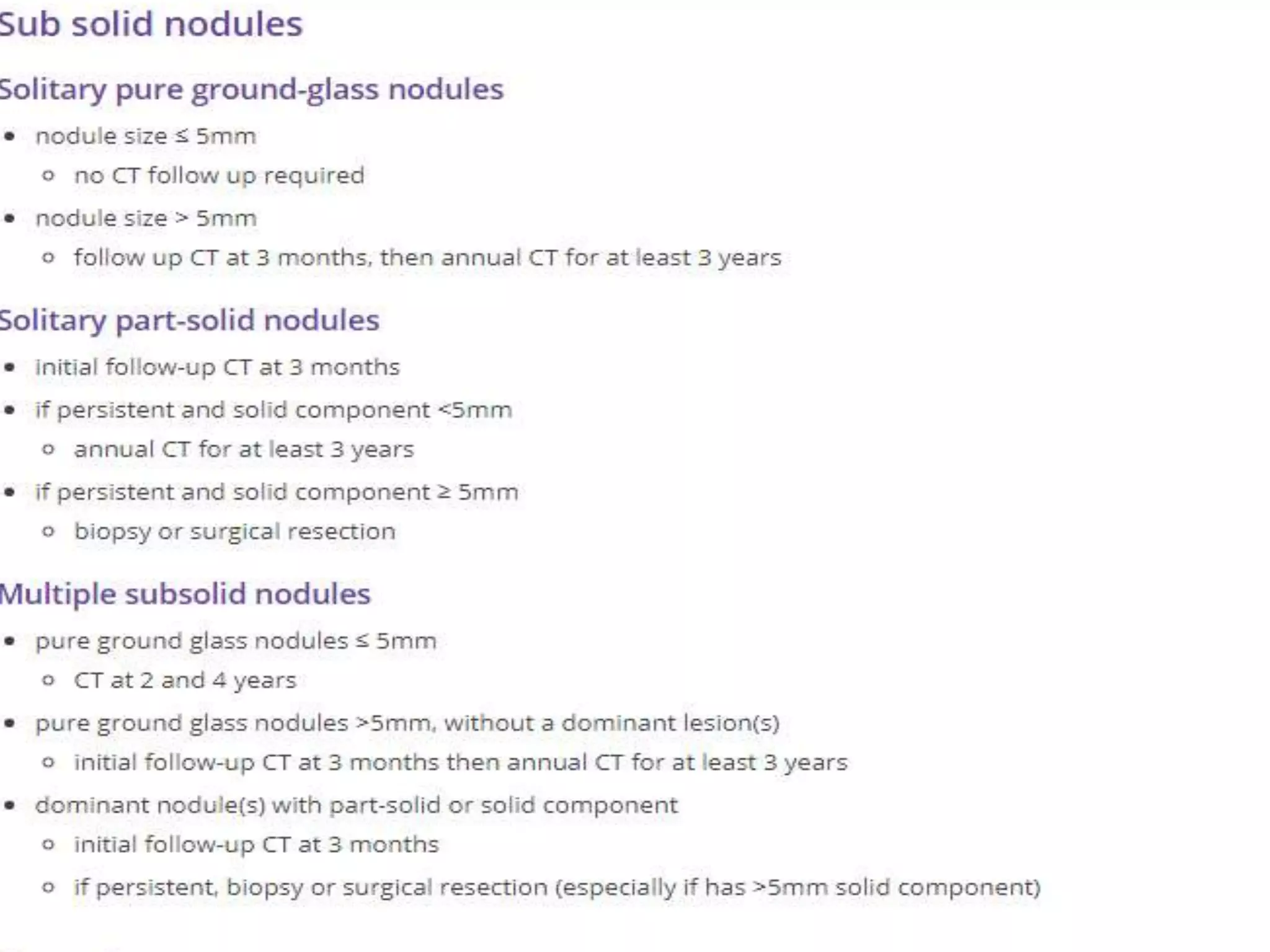
The document summarizes updated guidelines from the Fleischner Society for the management of incidental pulmonary nodules detected on CT images. Key changes include combining the previous separate guidelines for solid and subsolid nodules into a single simplified table. The guidelines provide recommendations for follow up examinations based on nodule size, type, risk factors and number of nodules detected. The purpose is to reduce unnecessary follow ups while allowing discretion for managing risk. The guidelines represent an international consensus to help evaluate pulmonary nodules and determine appropriate clinical response.