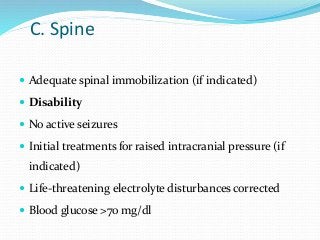
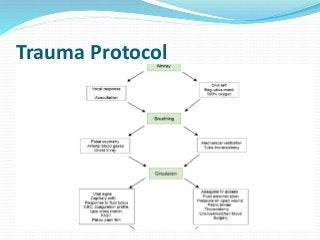
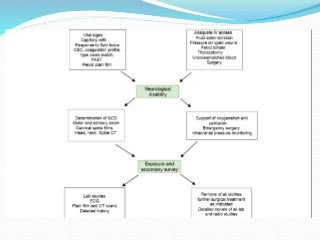
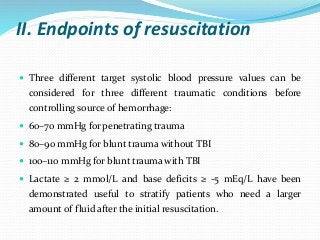
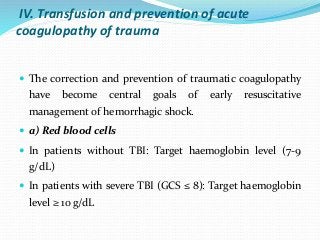
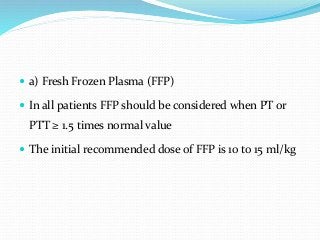
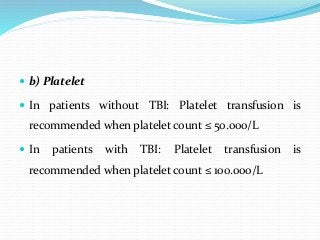
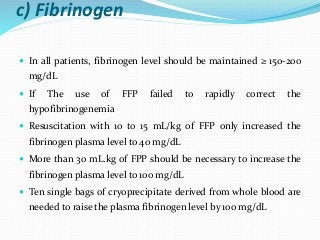
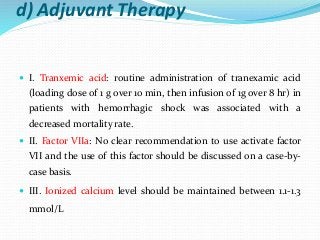
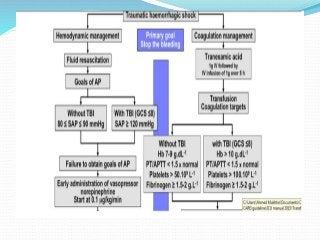
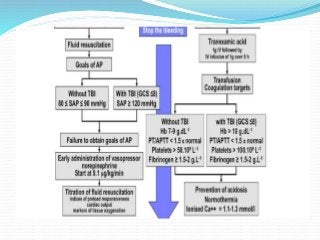
This document provides guidelines for trauma patient transfer and resuscitation protocols. It recommends that prior to transfer, patients with airway compromise should be intubated and ventilation should be stable on a transport ventilator. For circulation, intravenous access should be adequate and the patient should be hemodynamically stable. For trauma resuscitation, lactated Ringer's solution is recommended for fluid resuscitation. Target blood pressures for fluid resuscitation depend on trauma type. Early norepinephrine can limit fluid resuscitation and transfusion of blood products should aim to prevent traumatic coagulopathy.