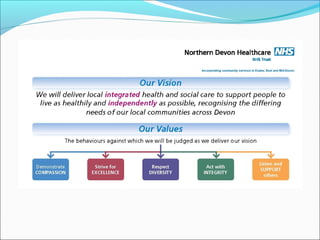
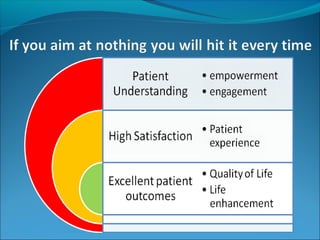
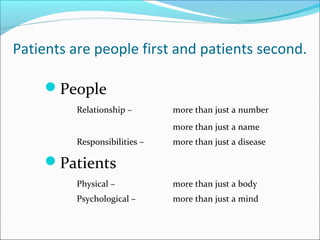
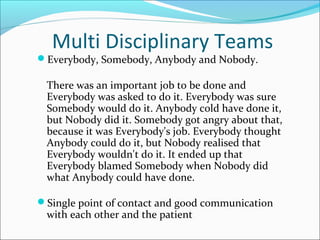
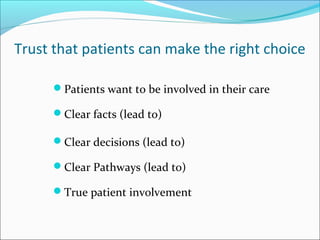
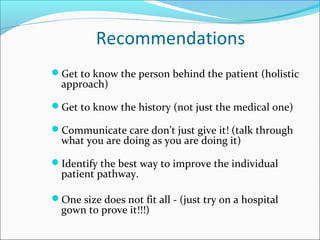
This document discusses promoting patient-centered care and perspectives. It emphasizes treating patients as people first by developing relationships, understanding their responsibilities beyond just their disease, and communicating clearly. It also stresses the importance of involving patients in their own care by providing clear facts, decisions, and pathways. Finally, it recommends getting to know the individual patient's history and needs in order to improve their care experience.