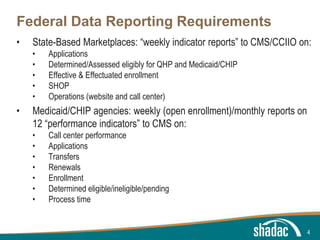
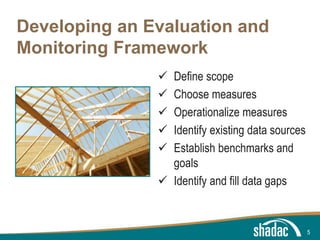
The document discusses the value of coordinating health care monitoring and reporting efforts across different state and federal programs. It outlines key components of developing an effective monitoring framework, including defining the scope, choosing measures, identifying data sources, and establishing benchmarks and goals. Coordinated monitoring can help provide a clear picture of reform impacts, avoid data discrepancies, and facilitate rapid response to changing policy needs.