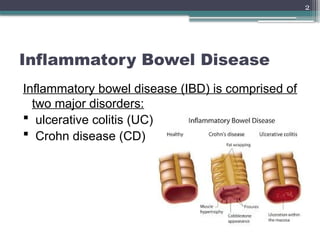
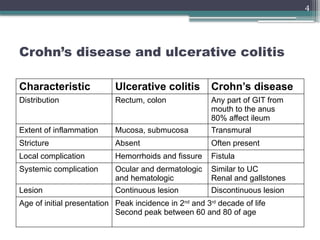
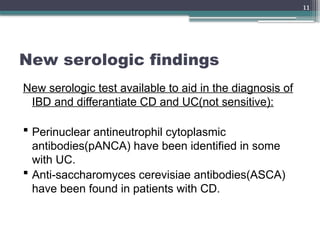
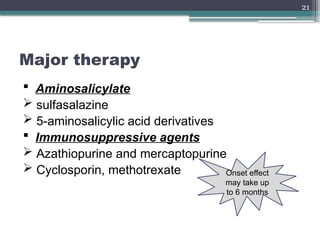
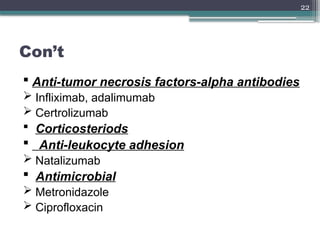
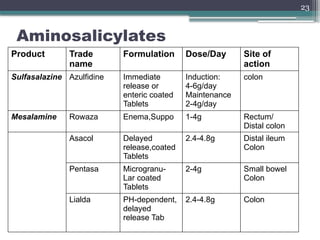
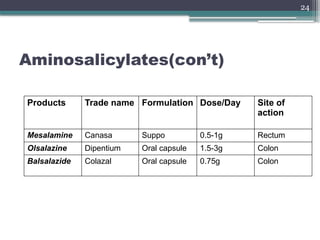
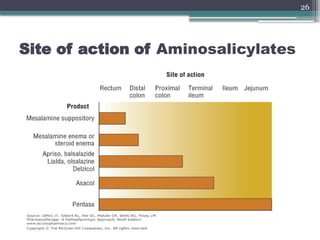
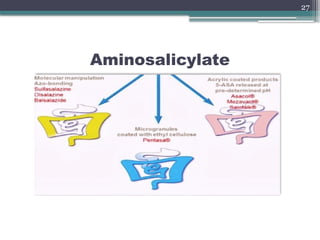
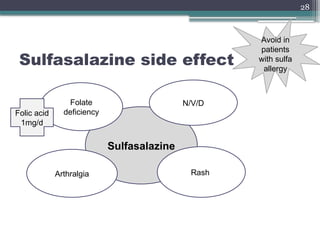
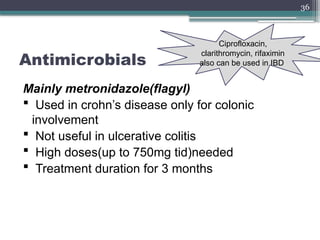
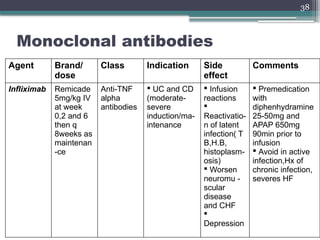
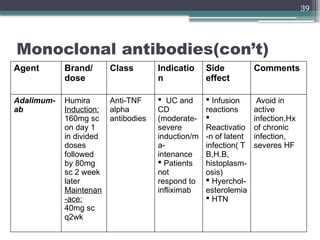
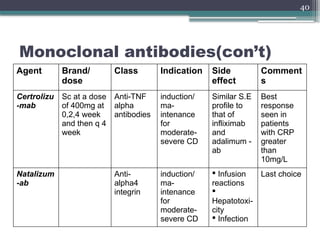
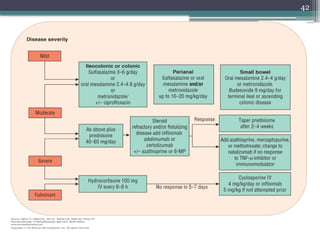
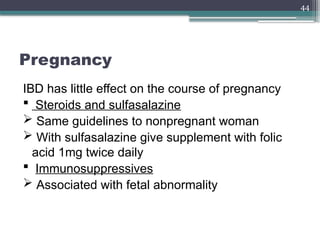
Inflammatory bowel disease (IBD) includes ulcerative colitis (UC) and Crohn's disease (CD), affecting different regions of the gastrointestinal tract with varying symptoms and complications. Diagnosis involves clinical presentation, stool examination, and imaging, while treatment options range from nutritional support to pharmacological therapies and surgery, depending on severity. Recent studies highlight the efficacy of new delivery systems for 5-ASA in achieving clinical remission in left-sided colitis.