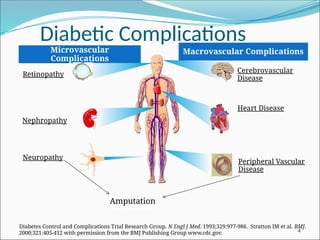
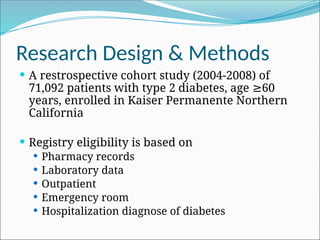
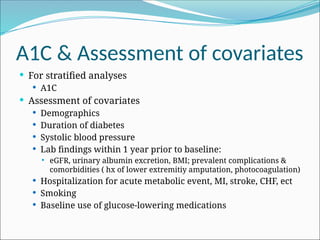
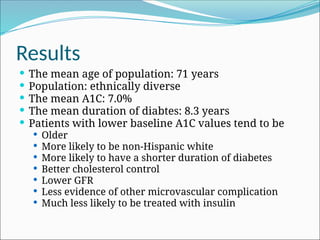
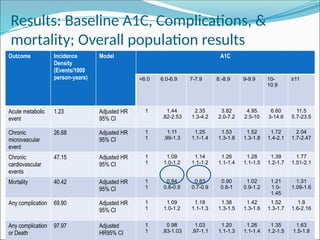
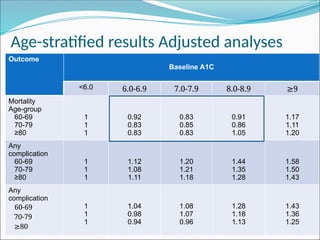
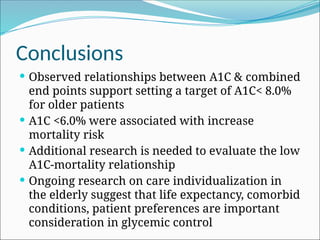
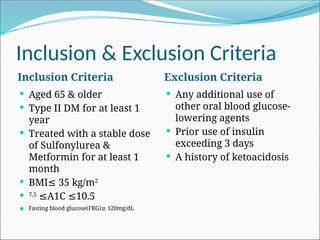
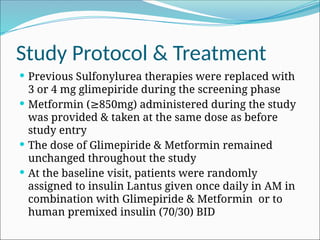
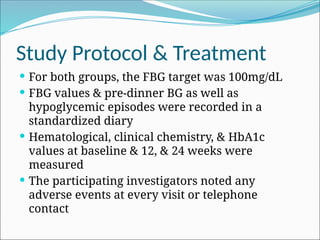
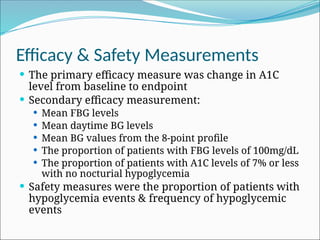
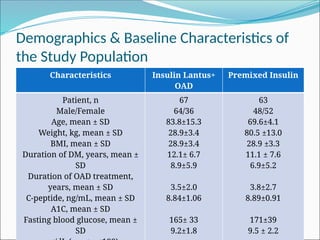
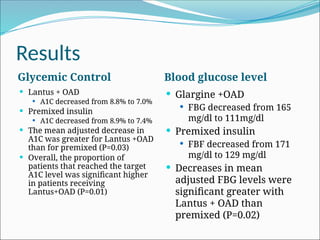
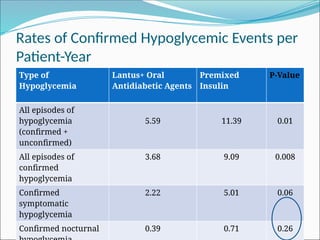
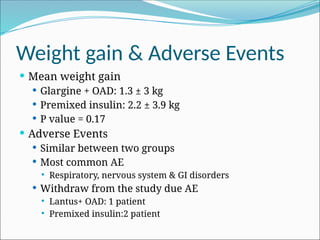
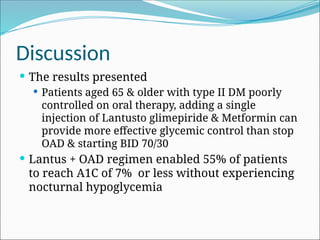
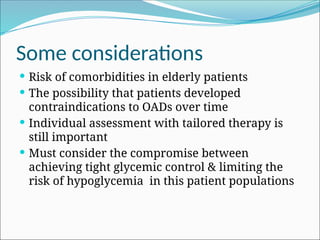
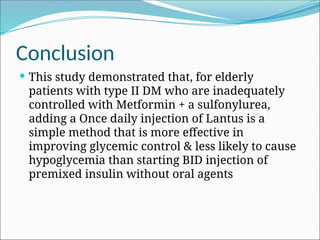
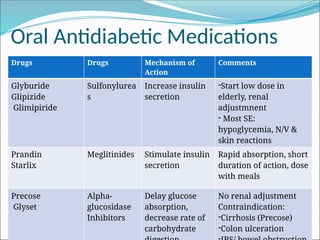
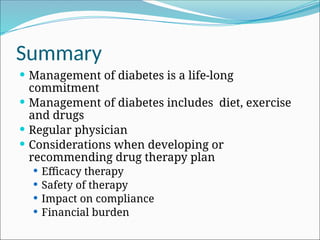
The document discusses diabetes management in elderly patients, focusing on glycemic control, complications, and treatment strategies. It presents findings from studies on optimal A1C targets for older adults and compares the effectiveness of insulin therapy regimens in improving glycemic control while minimizing hypoglycemia. The conclusion suggests a target A1C of <8.0% for older patients and highlights the advantages of adding insulin to oral agents over using premixed insulin alone.