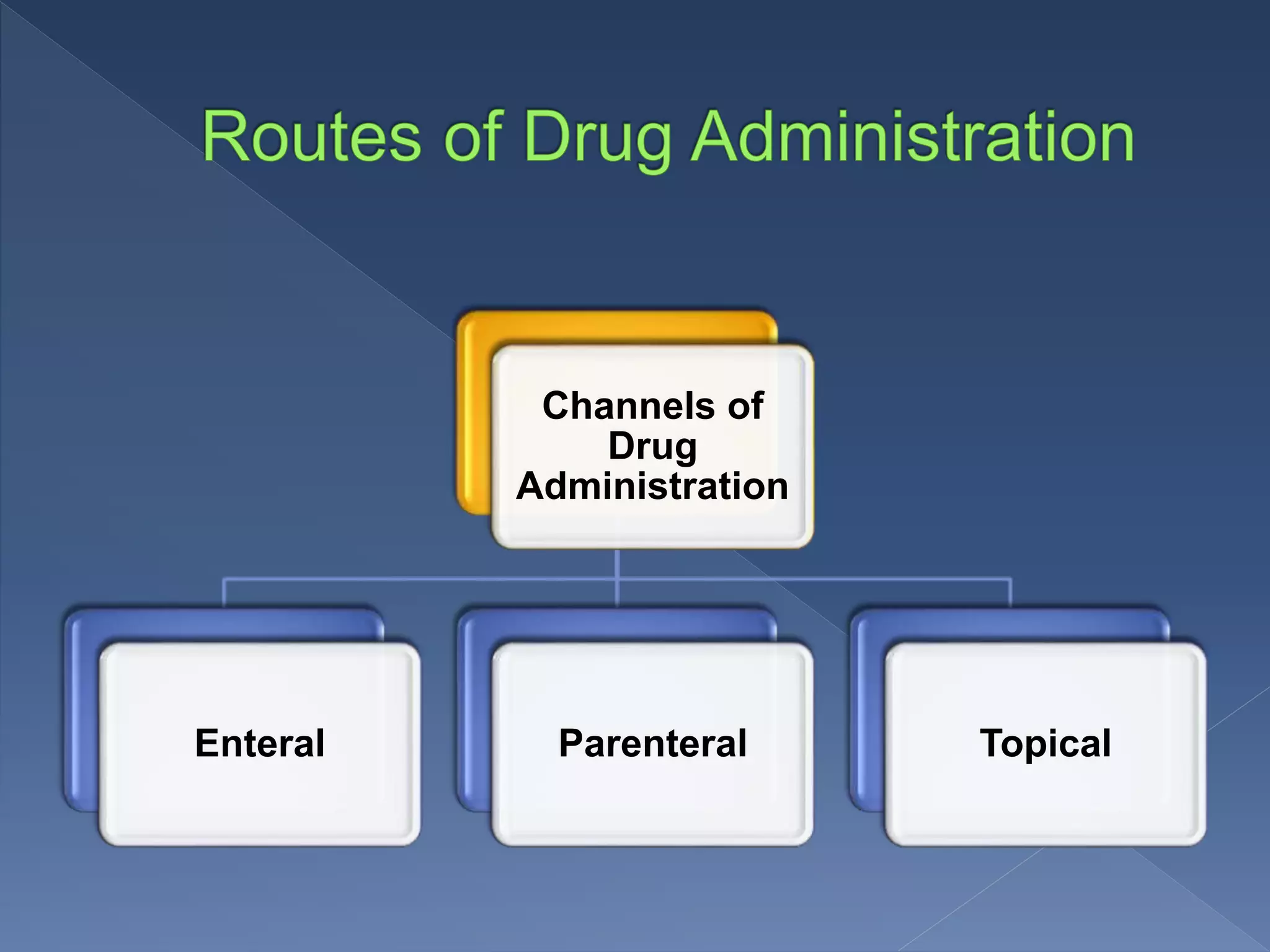
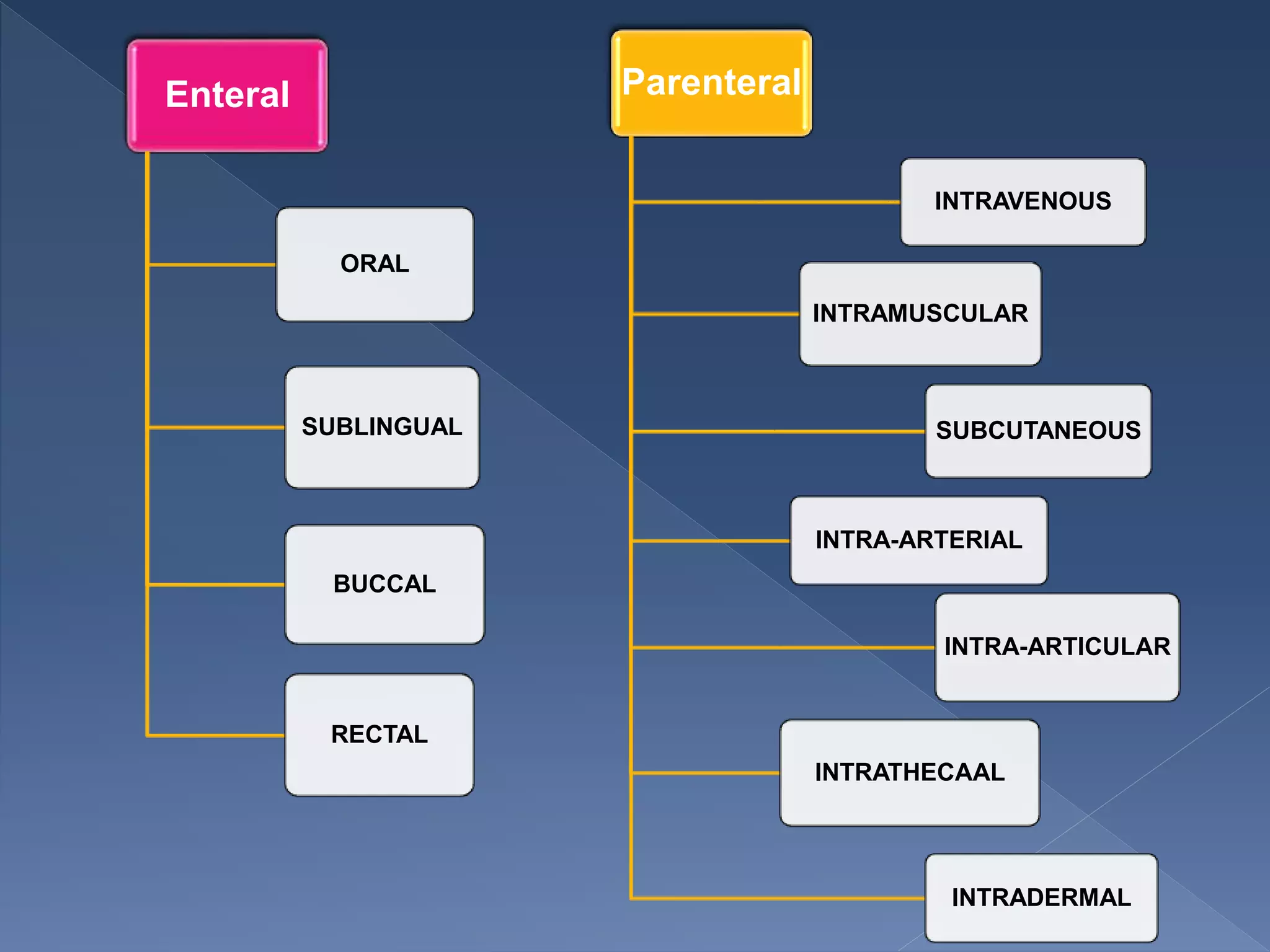
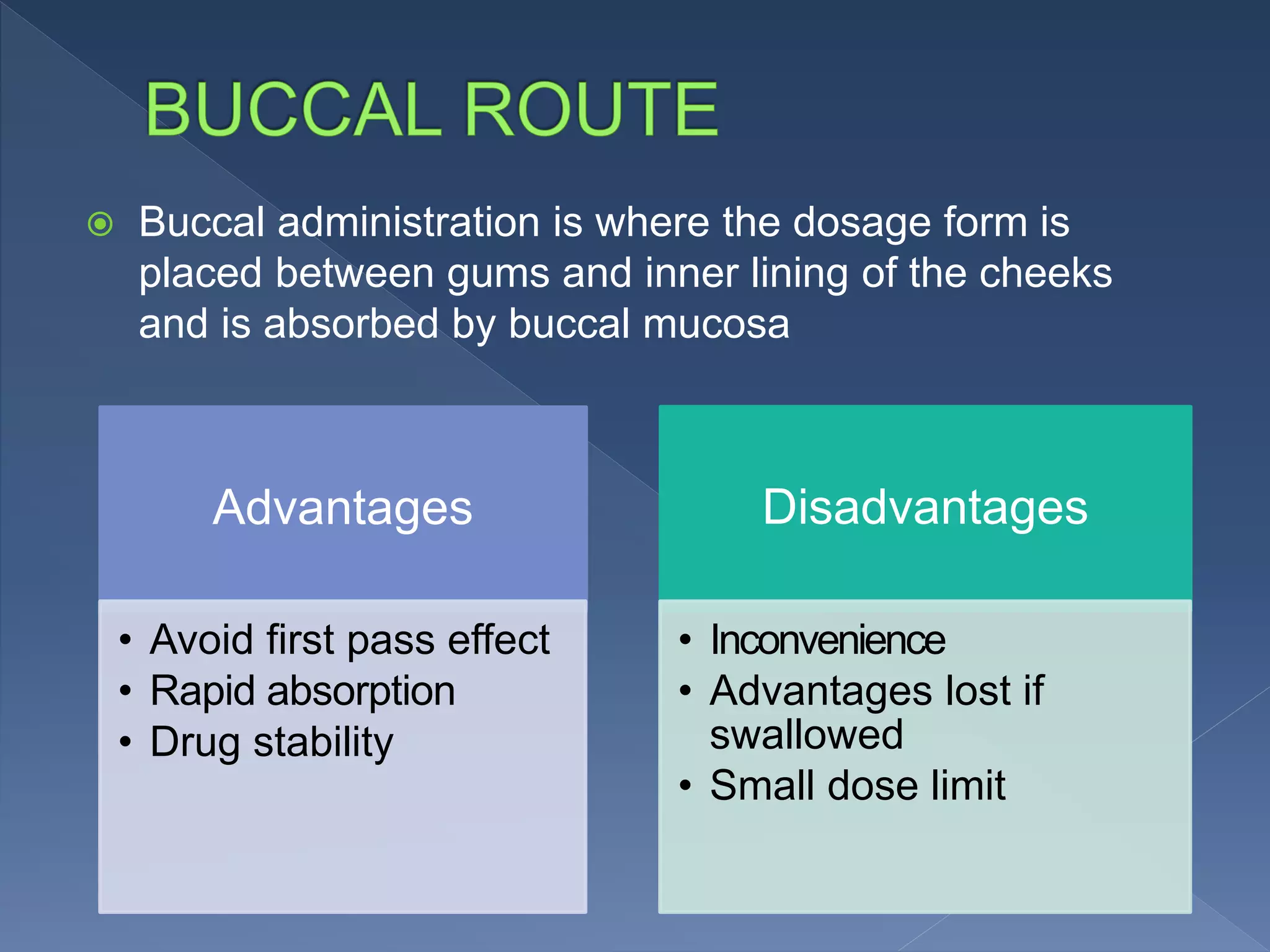
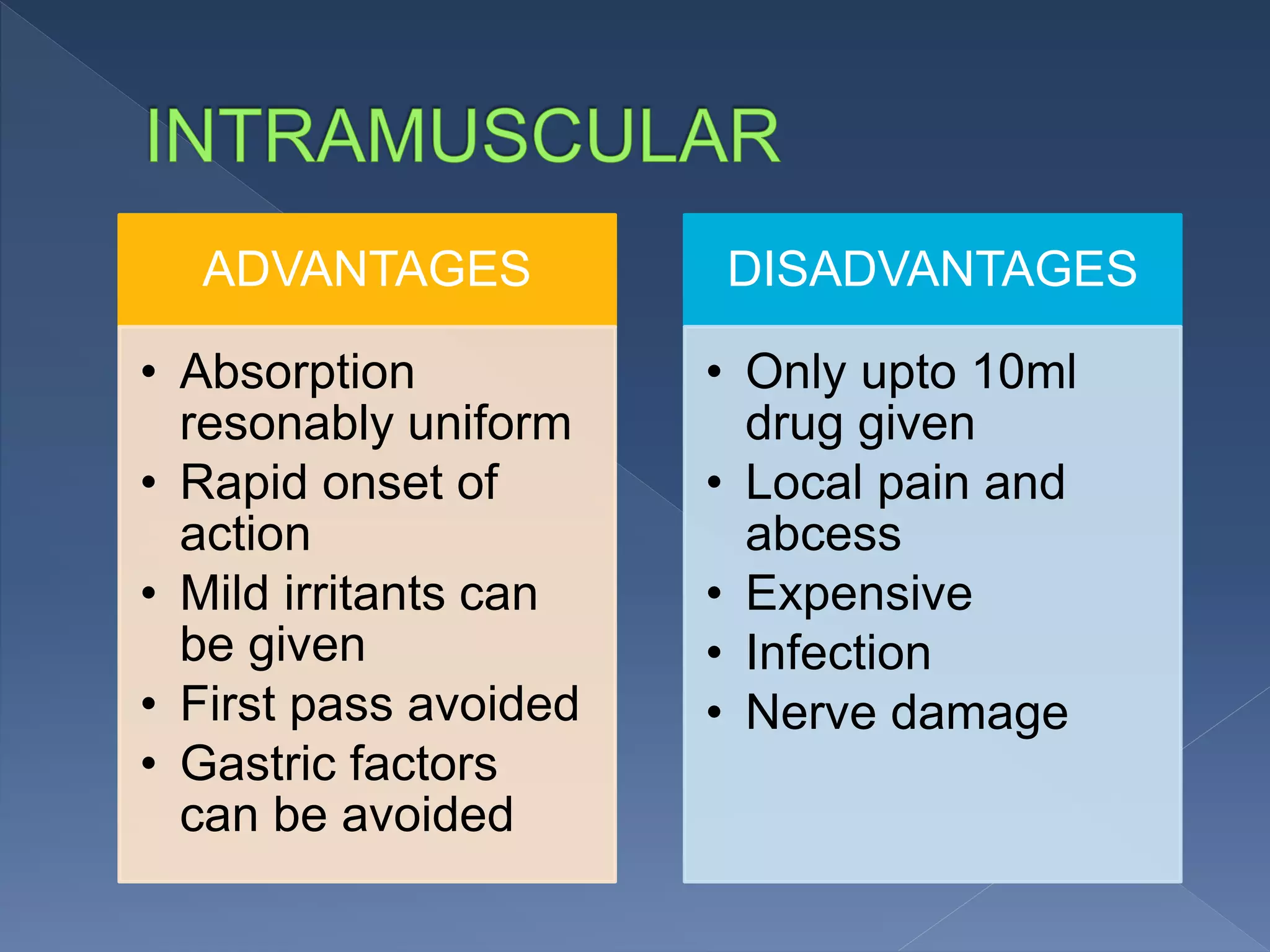
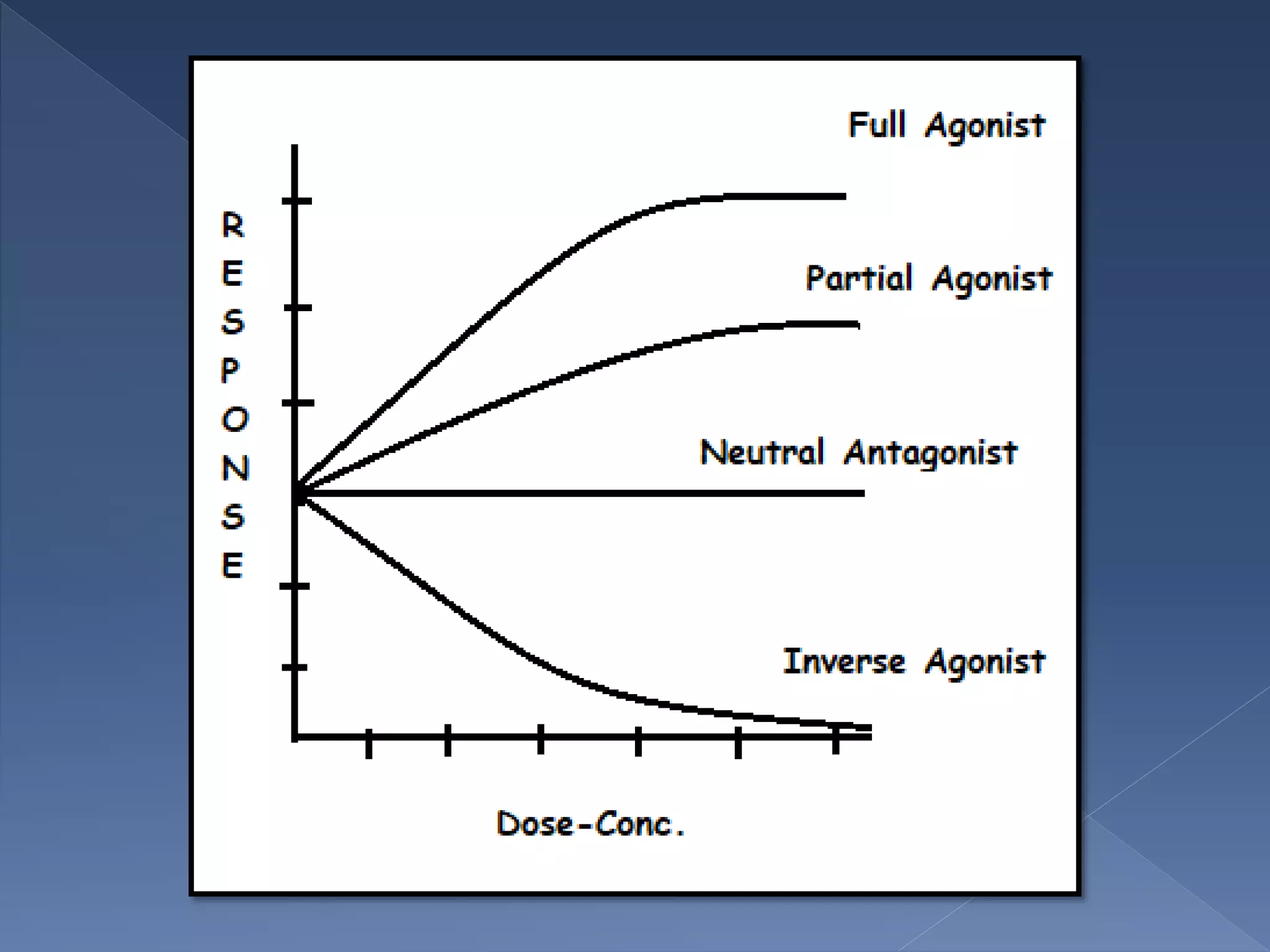
This document provides an overview of key concepts in pharmacology. It defines pharmacology and its branches, which include pharmacokinetics and pharmacodynamics. It discusses sources of drugs, routes of drug administration like oral, parenteral, and topical, and factors that determine administration route. It also covers ligands and their types like agonists and antagonists. In summary, the document outlines the fundamental principles of pharmacology including how drugs are developed, distributed in the body, and exert their effects.