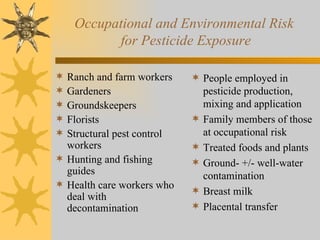
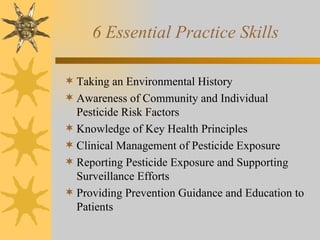
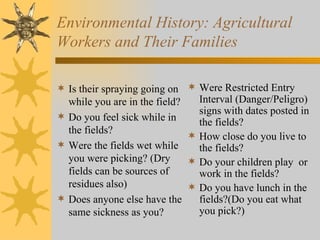
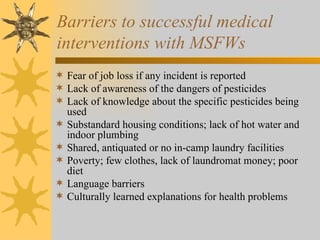
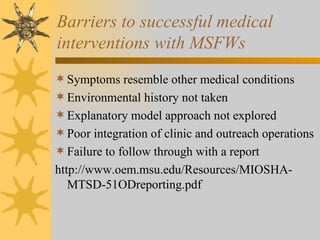
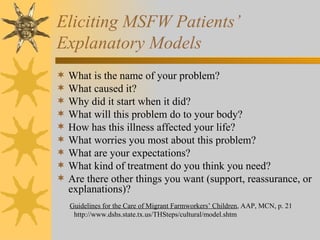
This document discusses the implications of pesticide exposure for migrant and community health centers. It notes that most medical professionals have not received education on pesticides during their training. It identifies populations at high risk for pesticide exposure and outlines six essential skills for healthcare providers in managing pesticide exposure cases, such as taking environmental histories and providing prevention education. Key barriers to care for migrant farmworkers are also discussed, such as fear of job loss and language/cultural barriers.