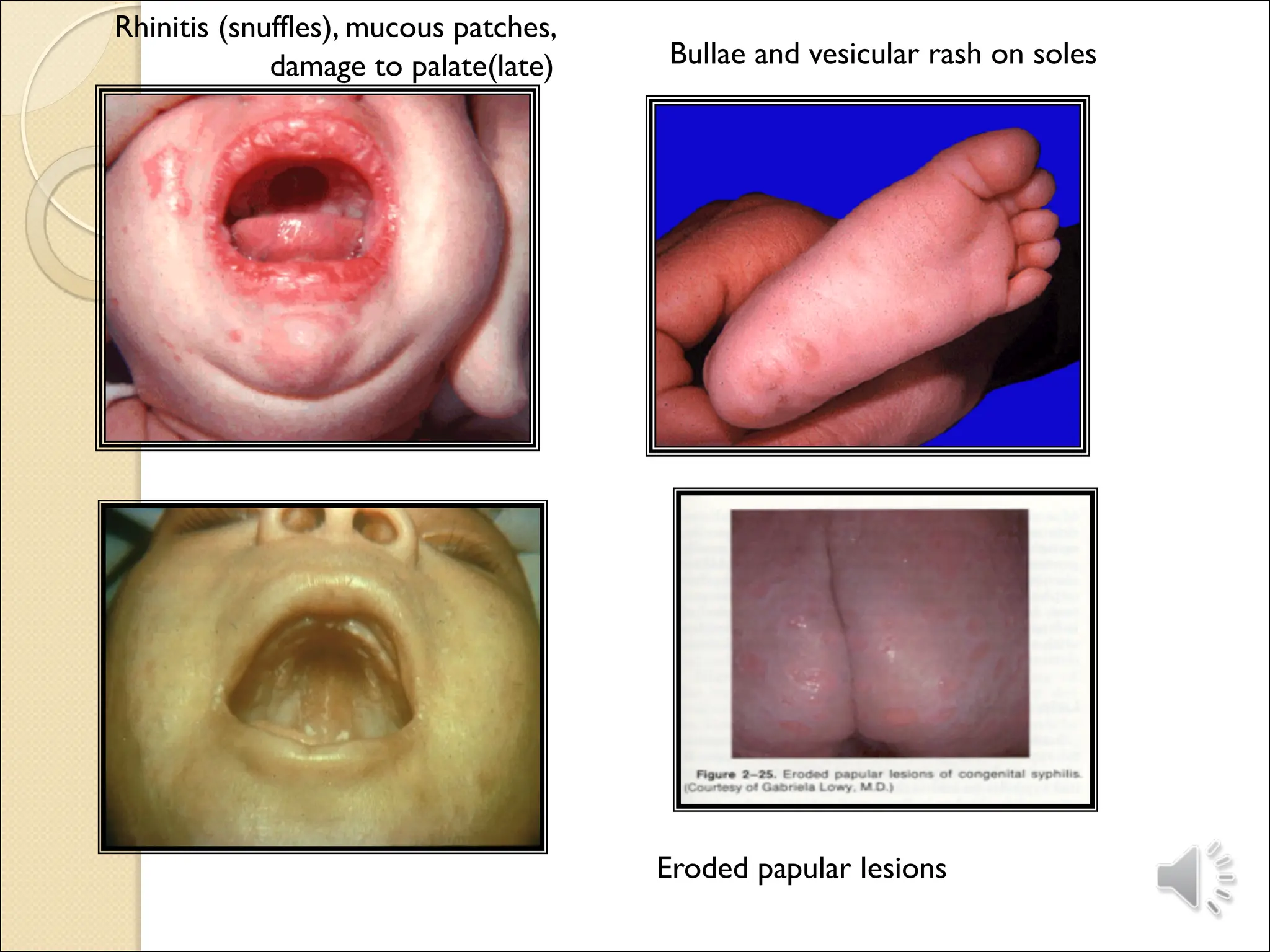
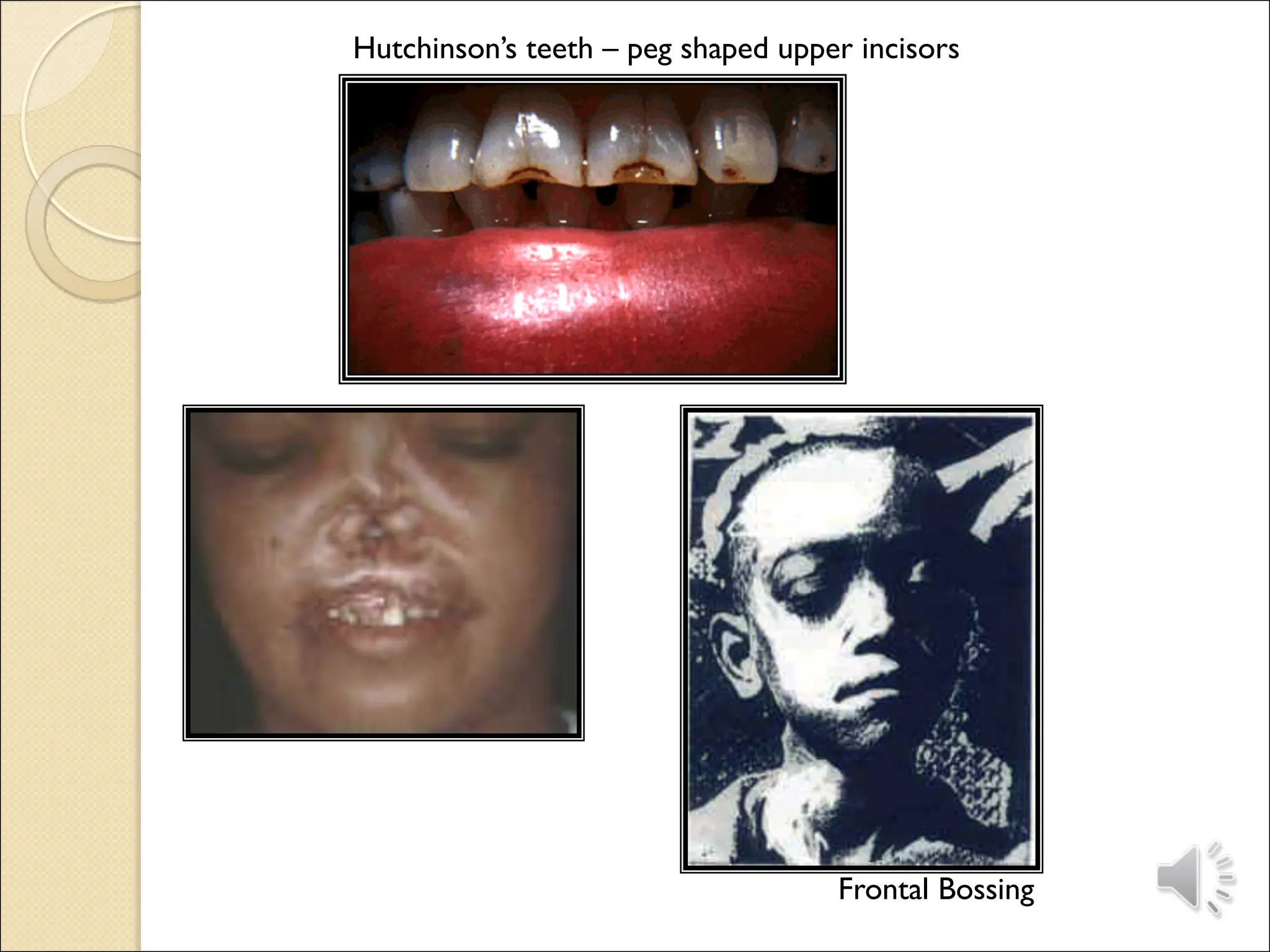
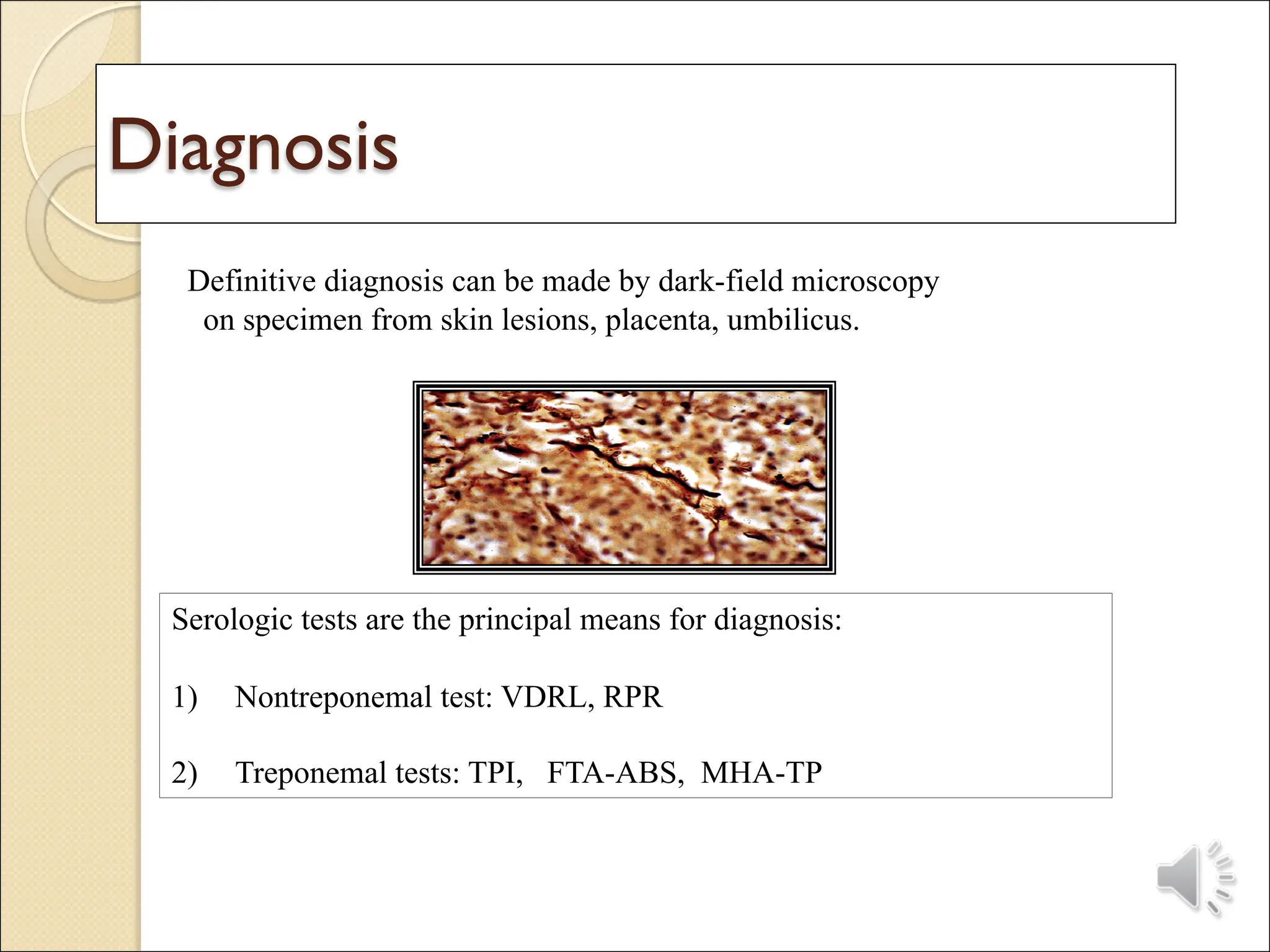
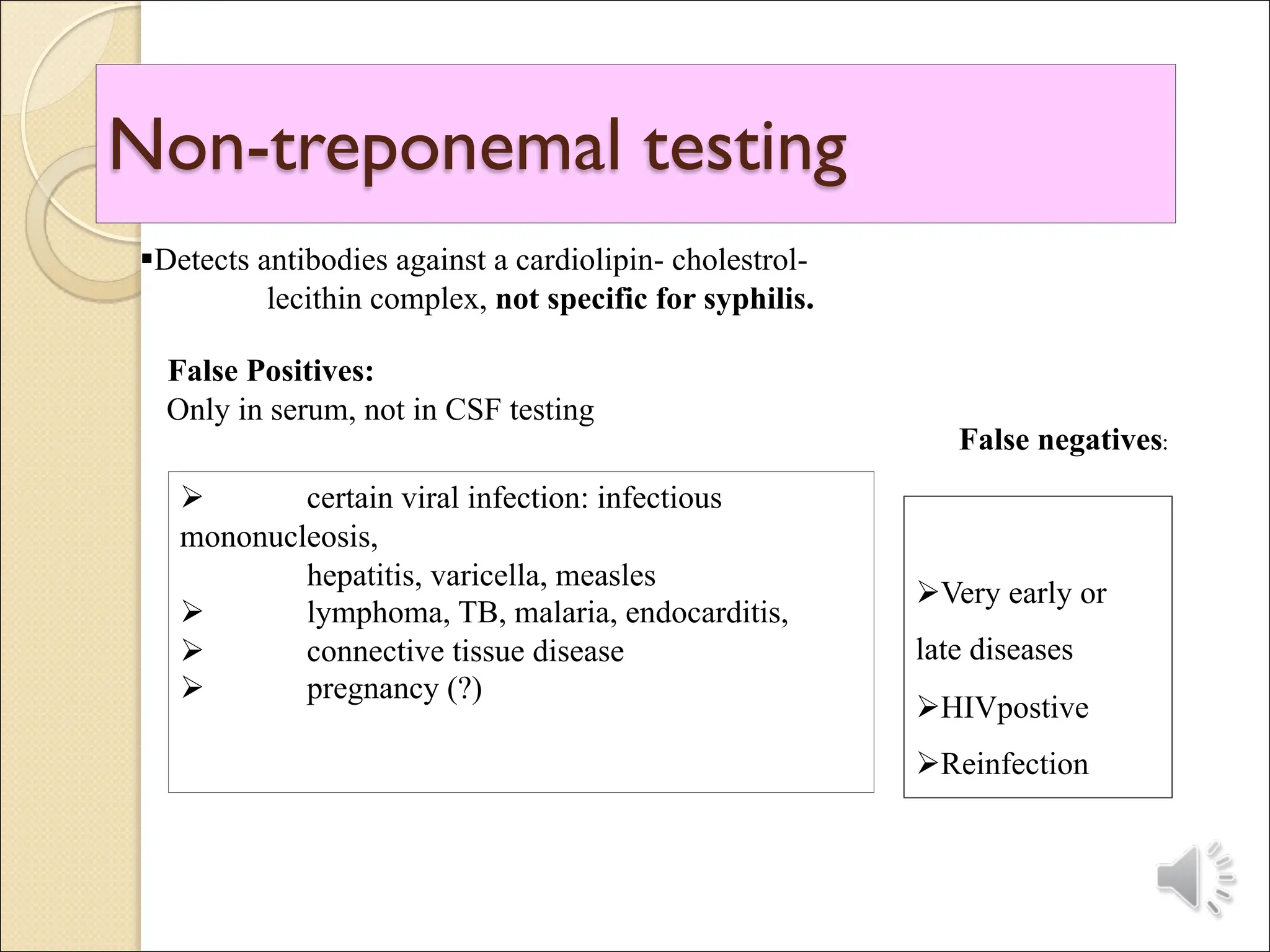
The document discusses perinatal infections, categorizing them into congenital infections leading to abnormalities, loss, or long-term disease, and infections occurring around delivery. It covers specific infections such as rubella, cytomegalovirus, chickenpox, syphilis, and toxoplasmosis, detailing their transmission, effects on the fetus, diagnosis, management, and prevention strategies. Each infection's risk to both the mother and the fetus is highlighted, emphasizing the importance of vaccination, screening, and timely medical interventions.