This document provides an overview of peptic ulcers, including:
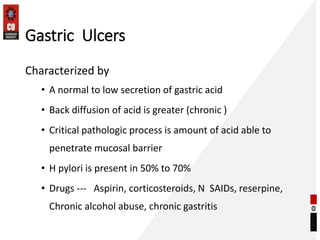
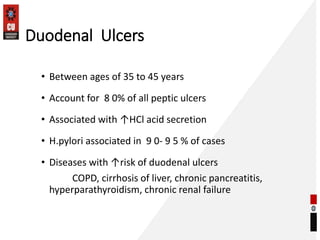
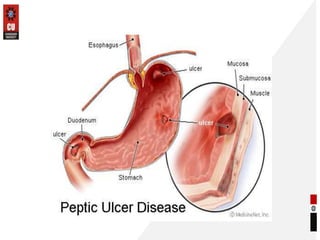
1. It defines peptic ulcers as erosions of the GI mucosa caused by digestive acids, most commonly occurring in the stomach and duodenum.
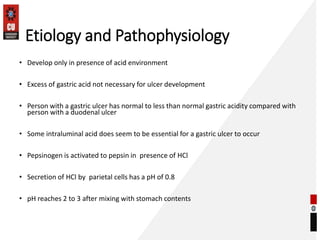
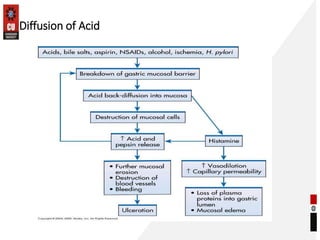
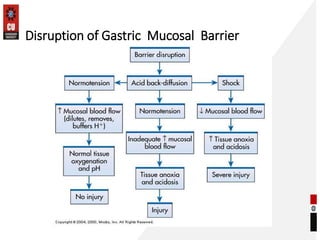
2. The pathophysiology of peptic ulcers is described as an imbalance between aggressive factors like acid and pepsin and protective mechanisms of the mucosa.
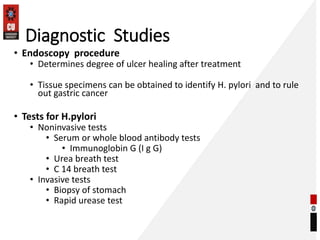
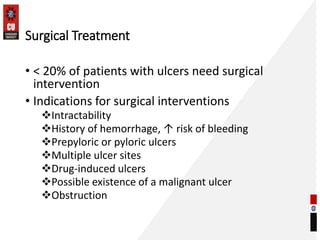
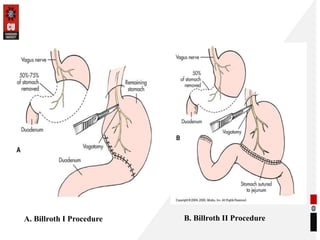
3. Treatment options for peptic ulcers include medications to reduce acid secretion, eradicate H. pylori infections, and surgery for complicated cases. Goals of treatment are to heal ulcers and prevent recurrence through lifestyle changes.




![TEXTBOOKS
T1 Vinay Kumar, Abul K. Abas, Jon C. Aster; Robbins & Cotran
Pathologic Basis of Disease; South Asia edition; India; Elsevier; 2014.
T2 Harsh Mohan; Text book of Pathology; 6th edition; India; Jaypee
Publications; 2010.
REFERENCE BOOKS
R1Laurence B, Bruce C, Bjorn K. ; Goodman Gilman’s The
Pharmacological Basis of Therapeutics; 12th edition; New York;
McGrawHill; 2011.
R2Best, Charles Herbert 1899-1978; Taylor, Norman Burke 1885-1972;
West, John B (John Burnard); Best and Taylor’s Physiological
basis of medical practice; 12th ed; united states
R3William and Wilkins, Baltimorec 1991 [1990 printing]
chandigarh university](https://image.slidesharecdn.com/pepticulcers-230517164747-5aecf6ed/85/Peptic-ulcers-pptx-27-320.jpg)