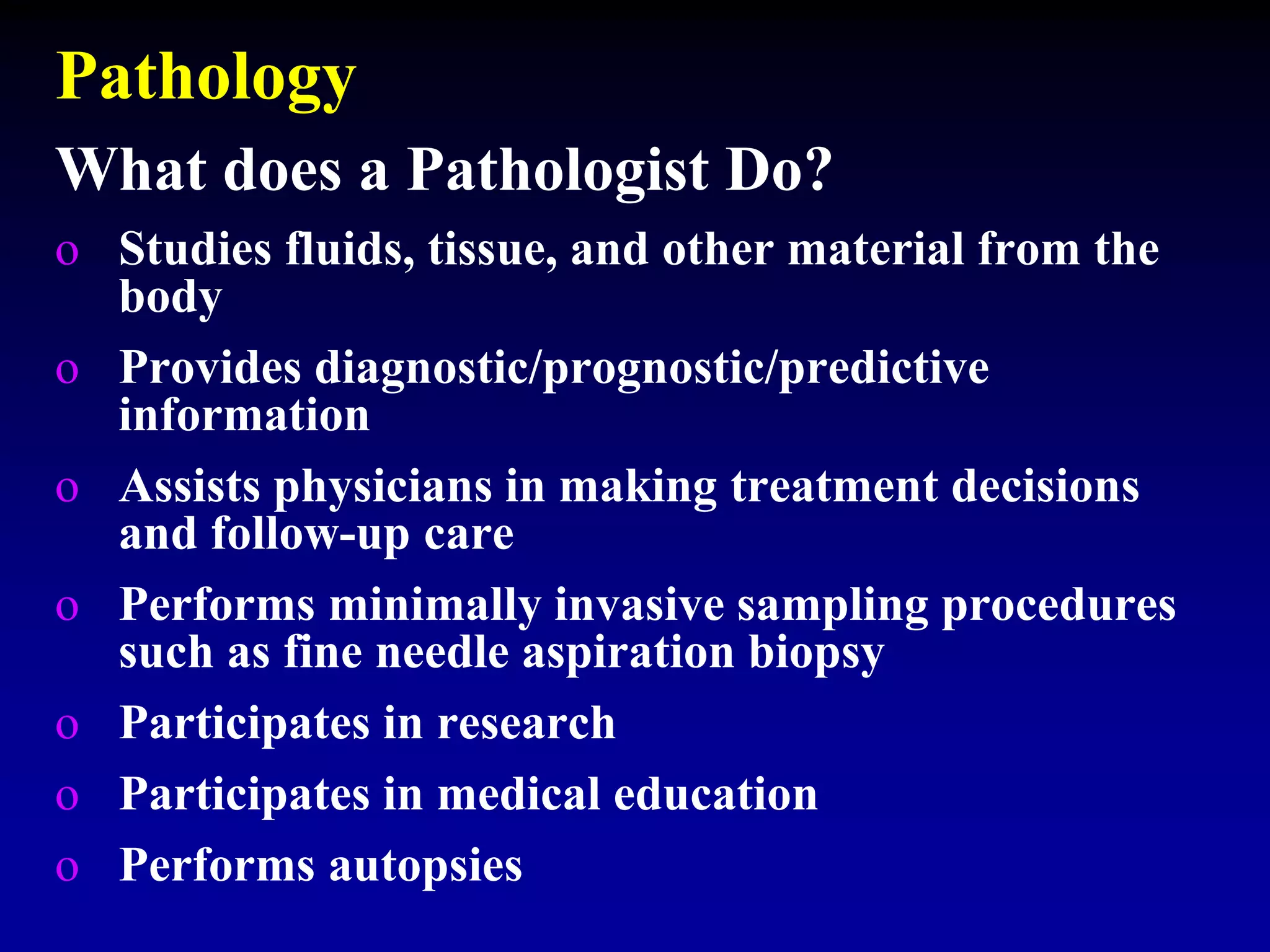
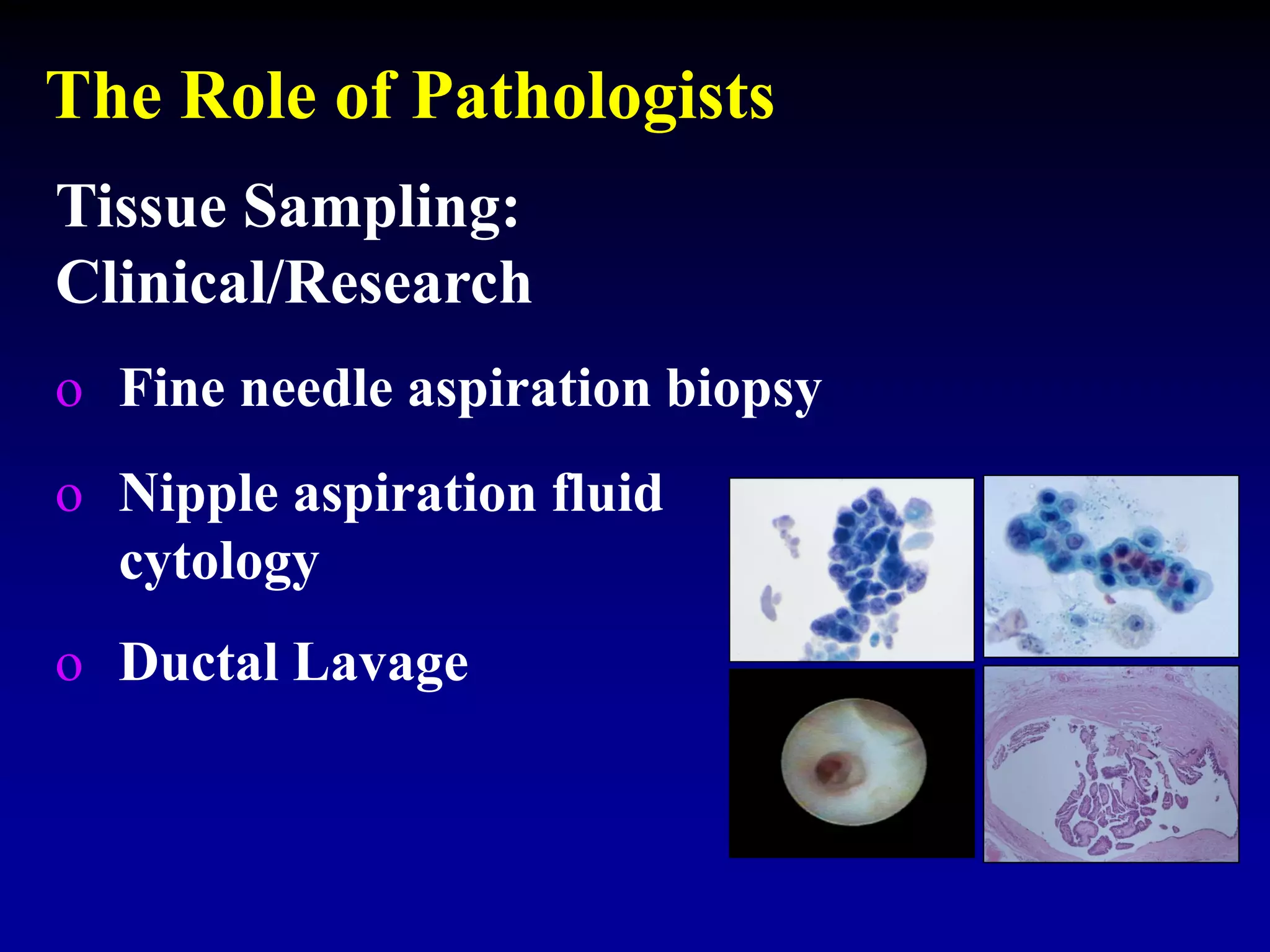
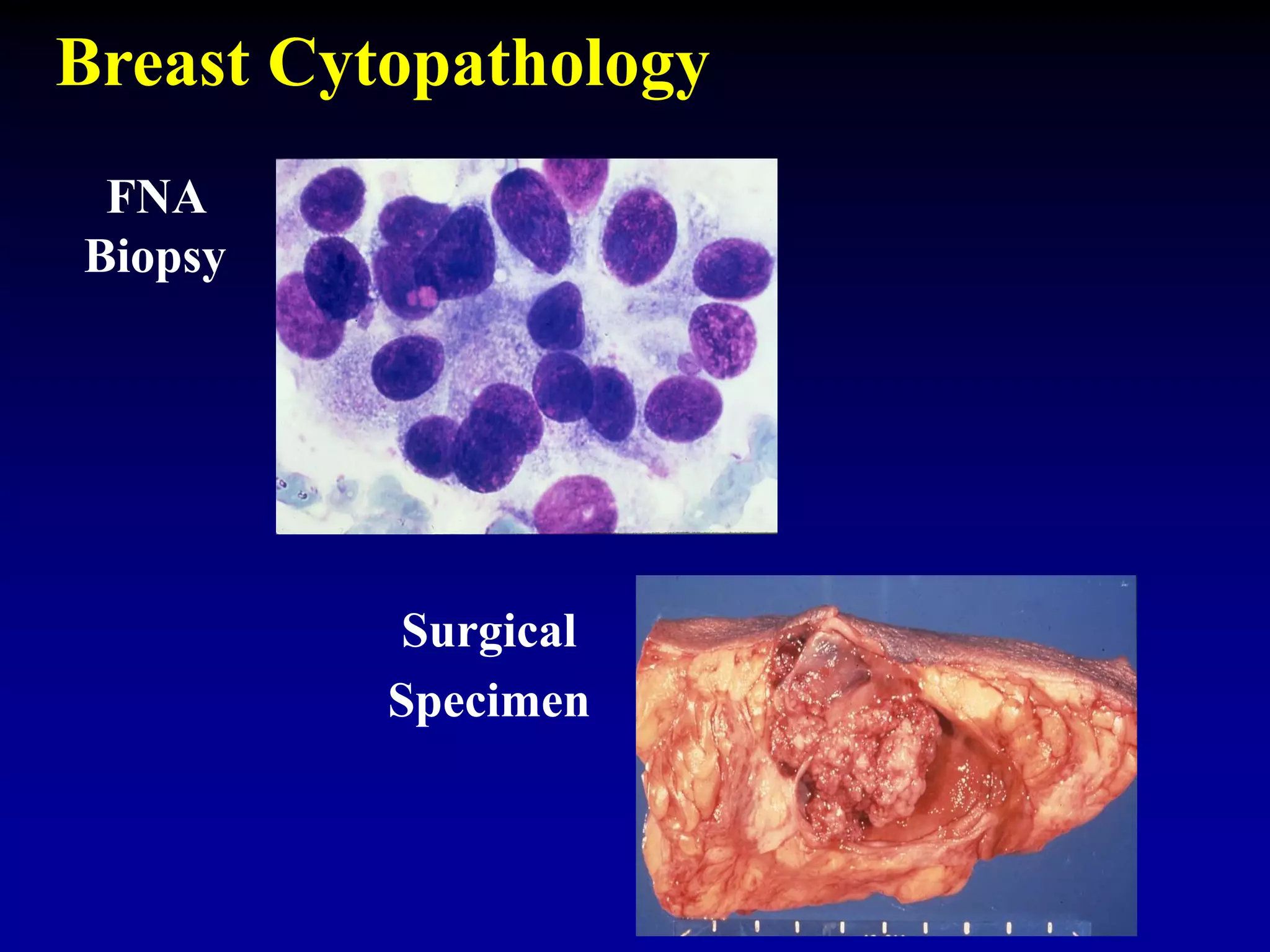
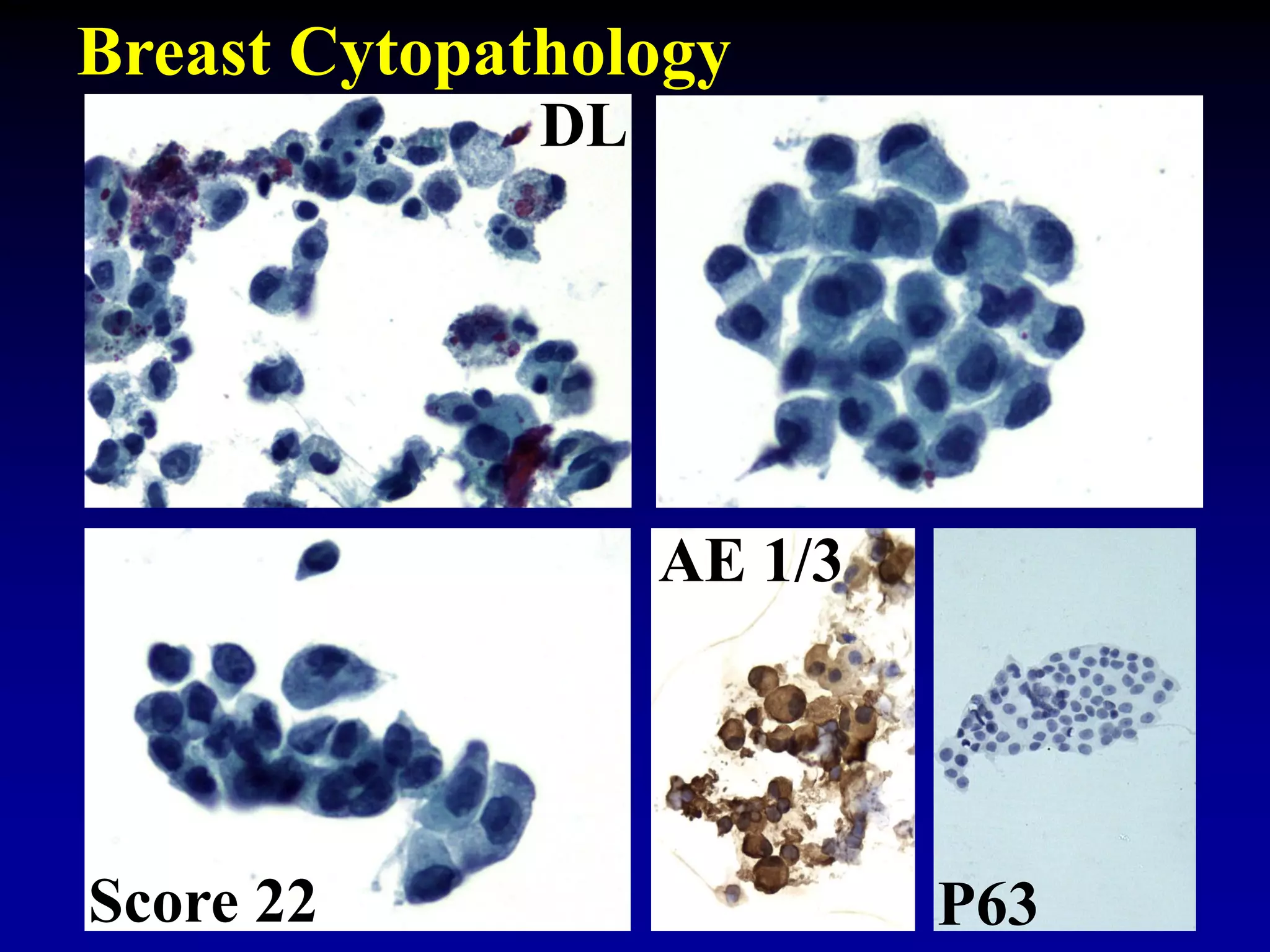
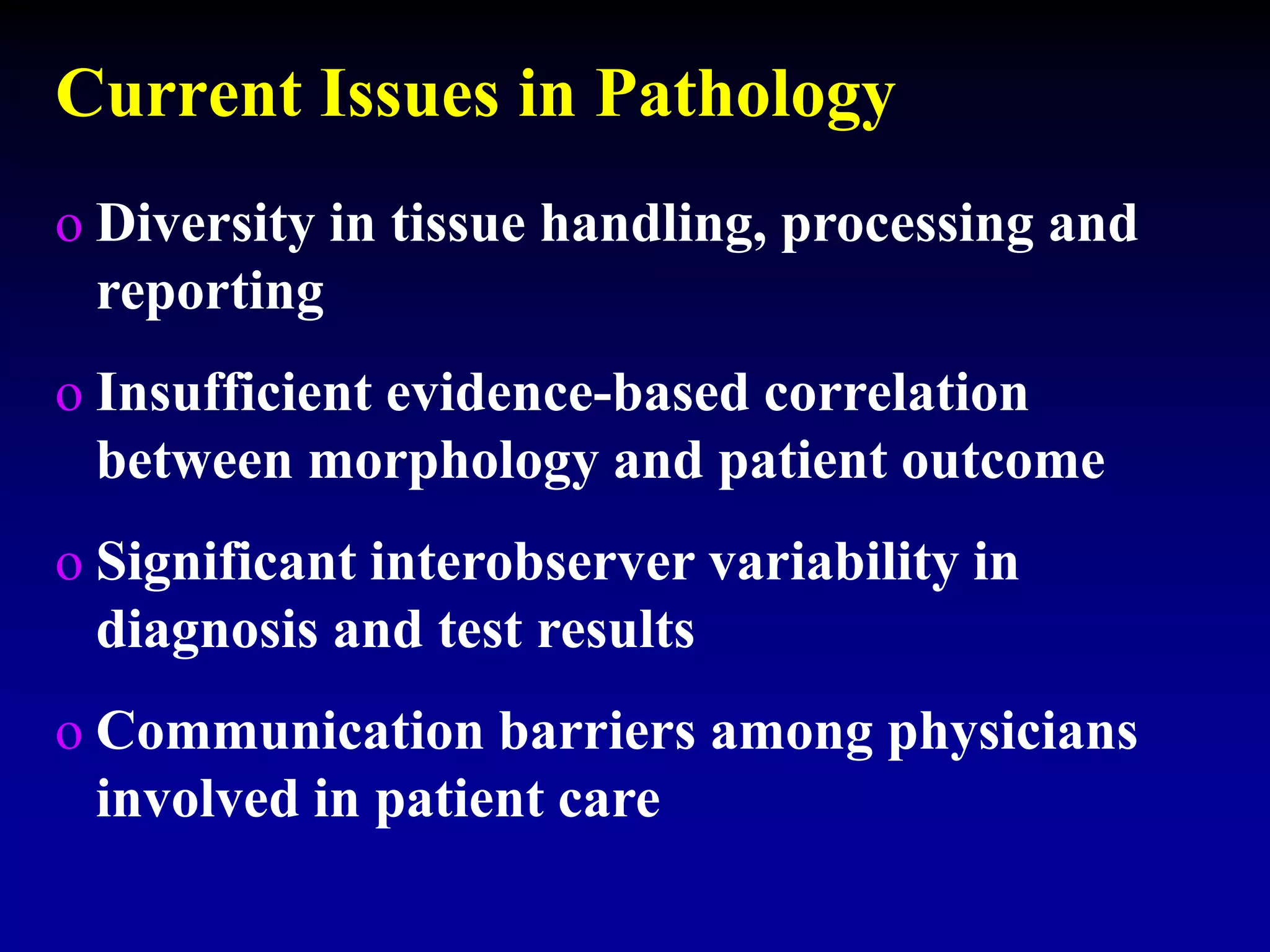
- Pathology plays a key role in patient diagnosis, treatment decisions, and outcomes through tissue examination and ancillary studies.
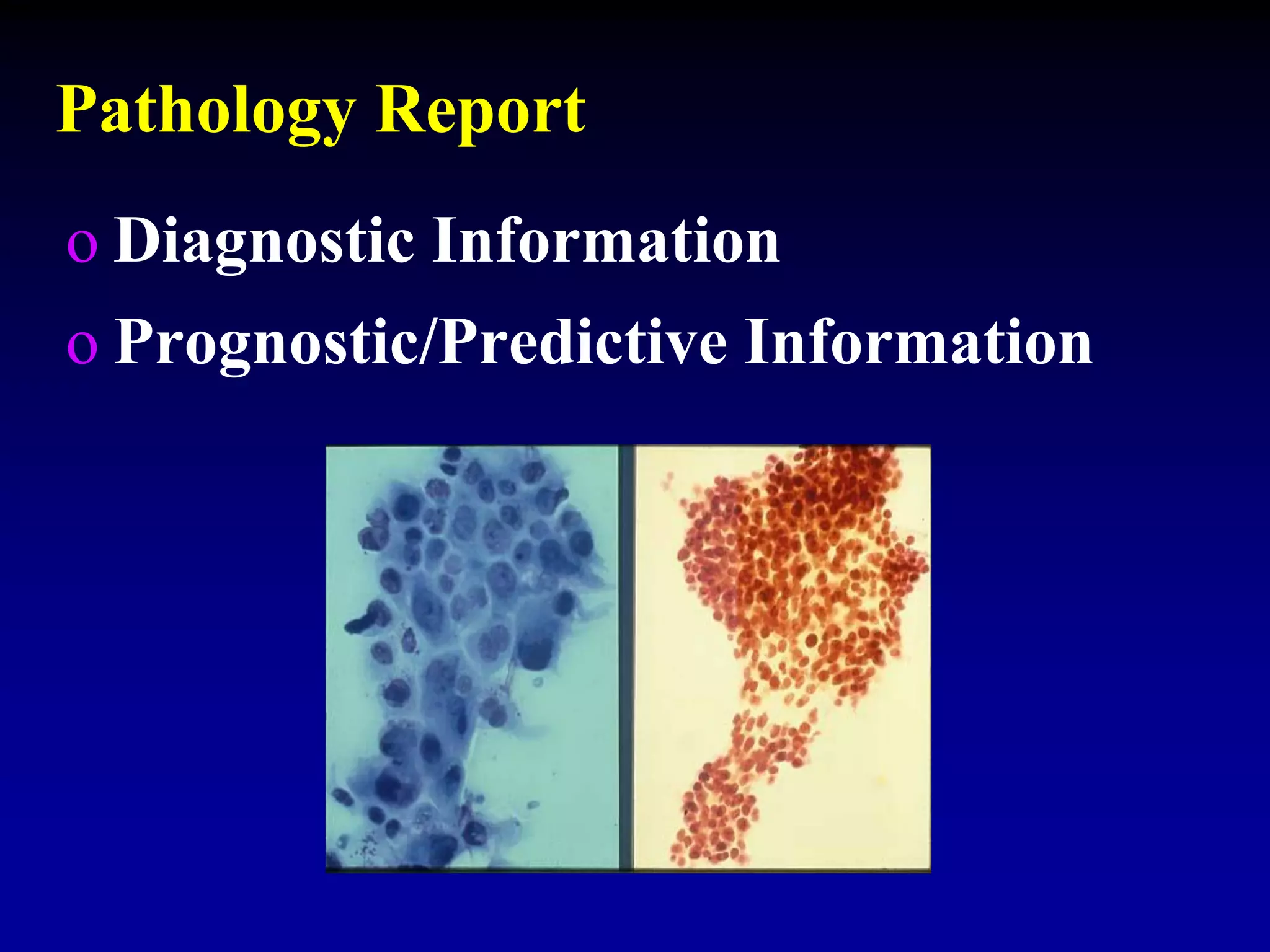
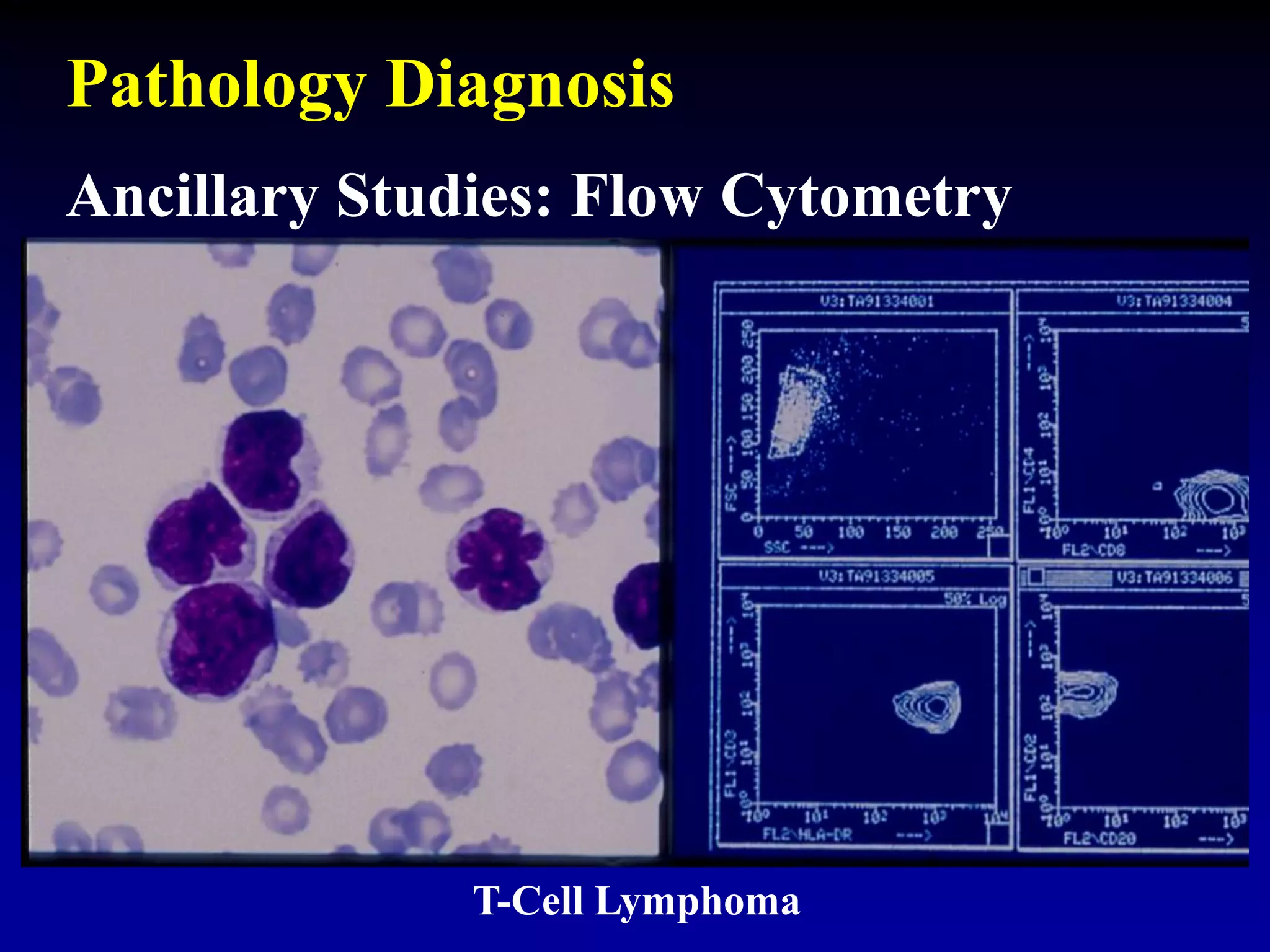
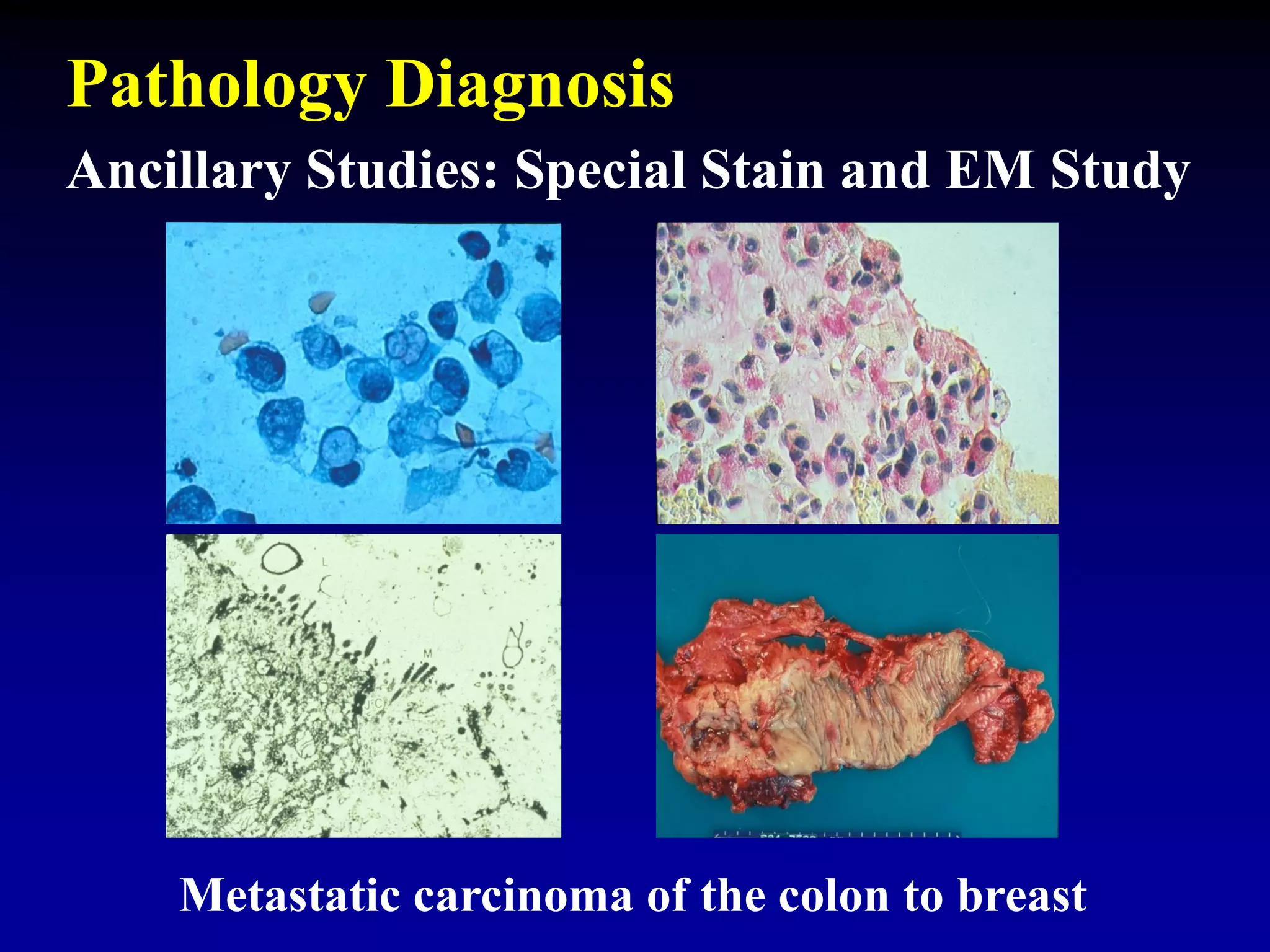
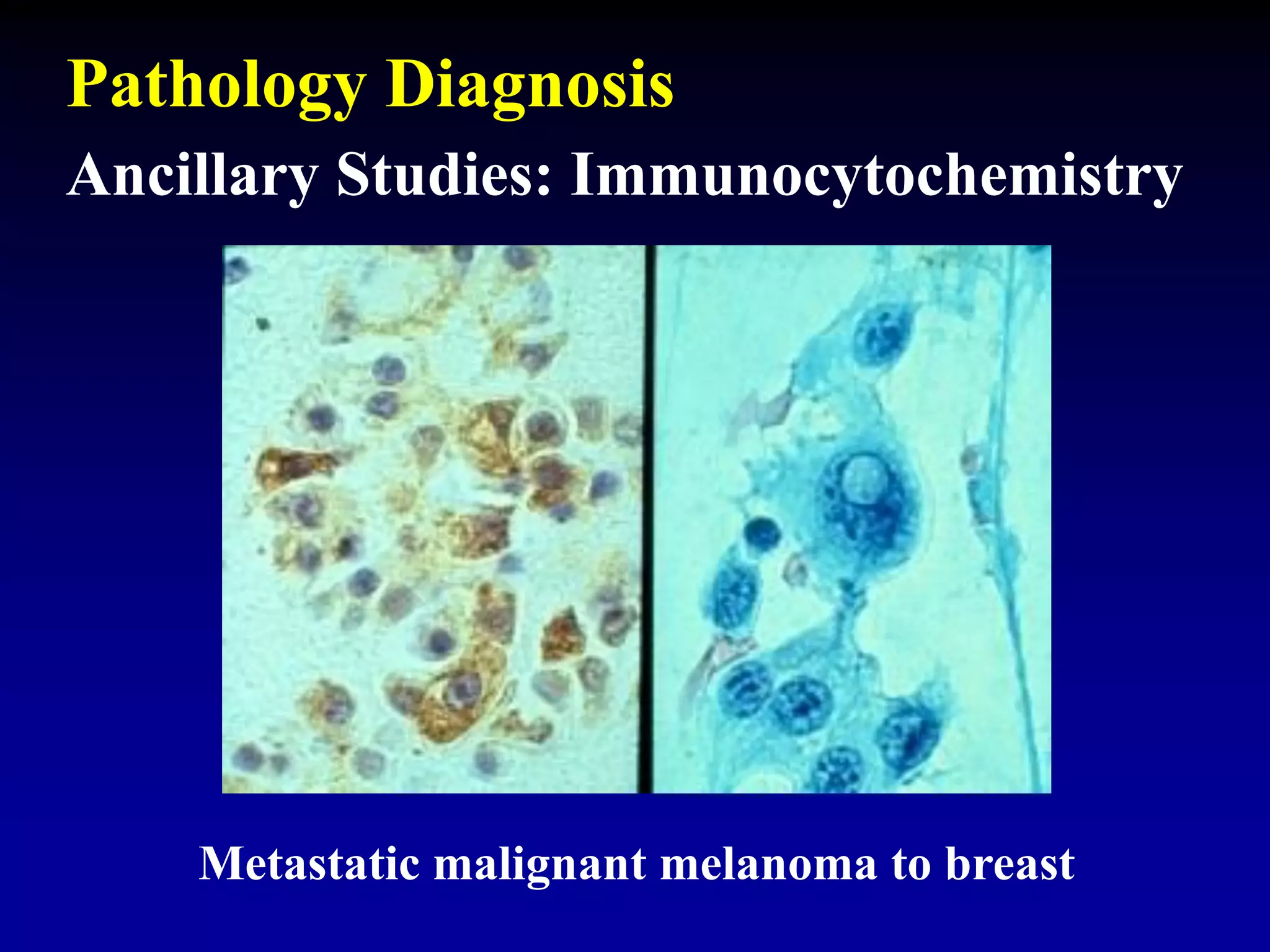
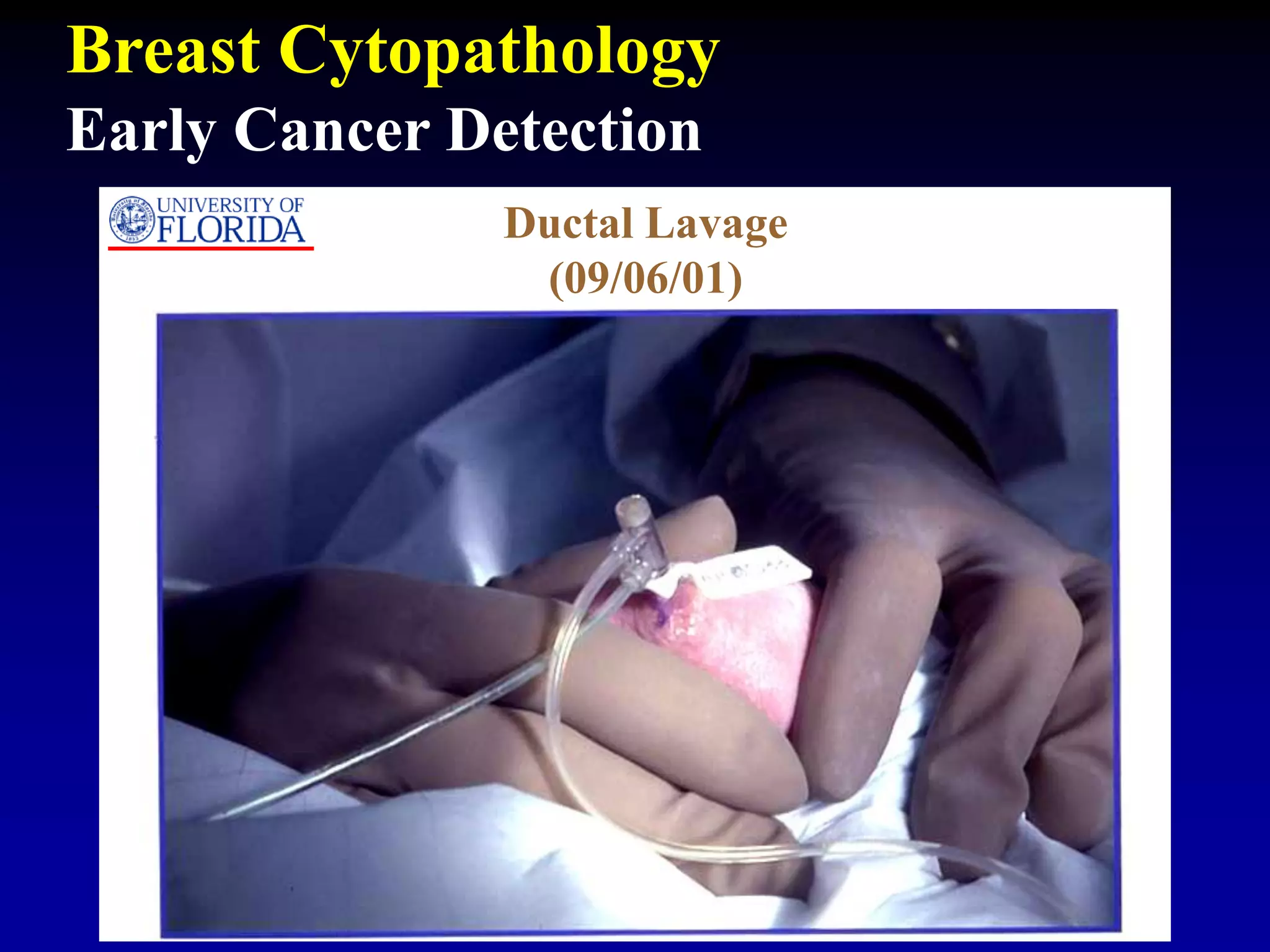
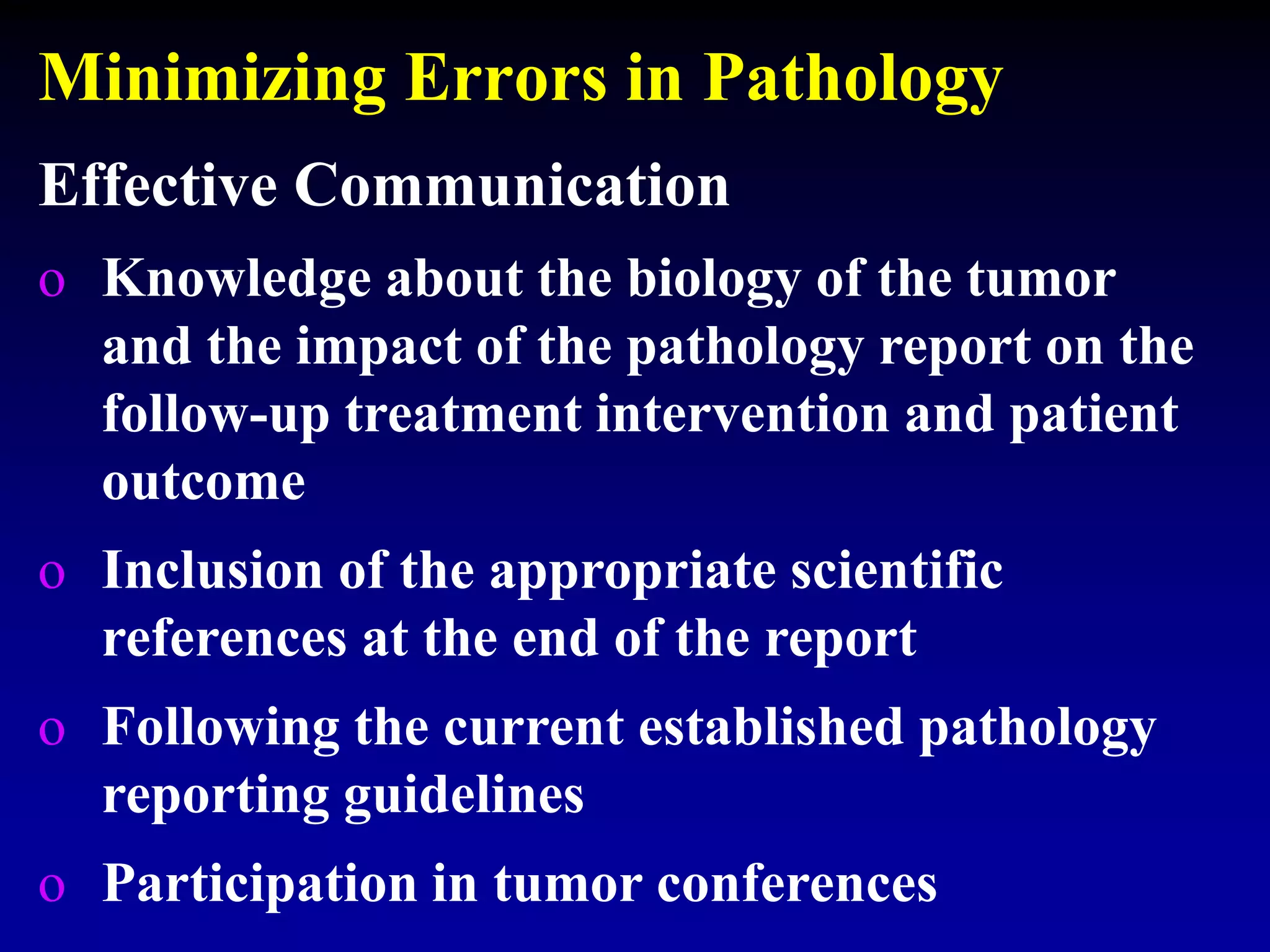
- A pathologist's report provides the diagnosis, prognostic/predictive factors, and assists physicians. New technologies have improved characterization.
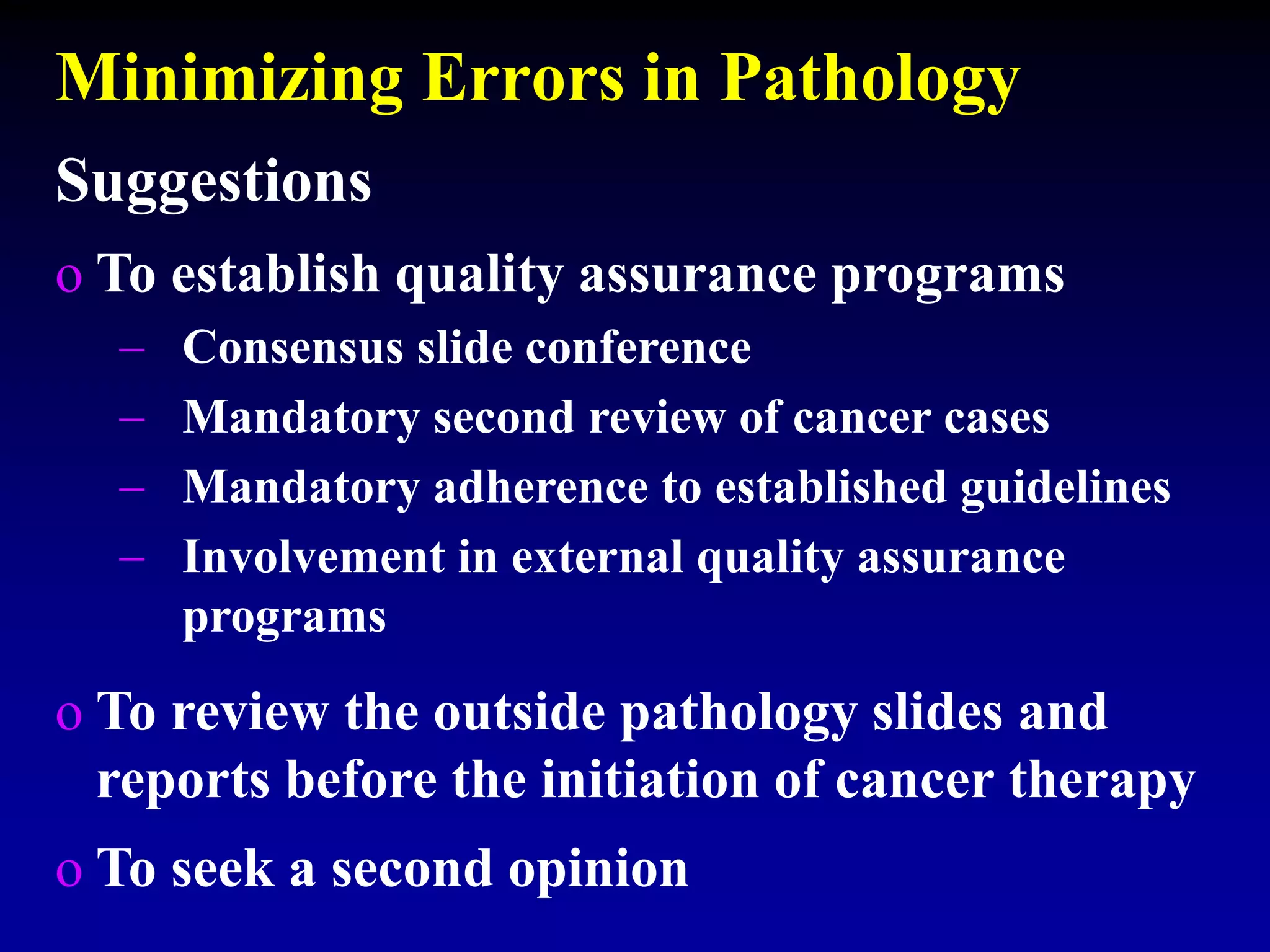
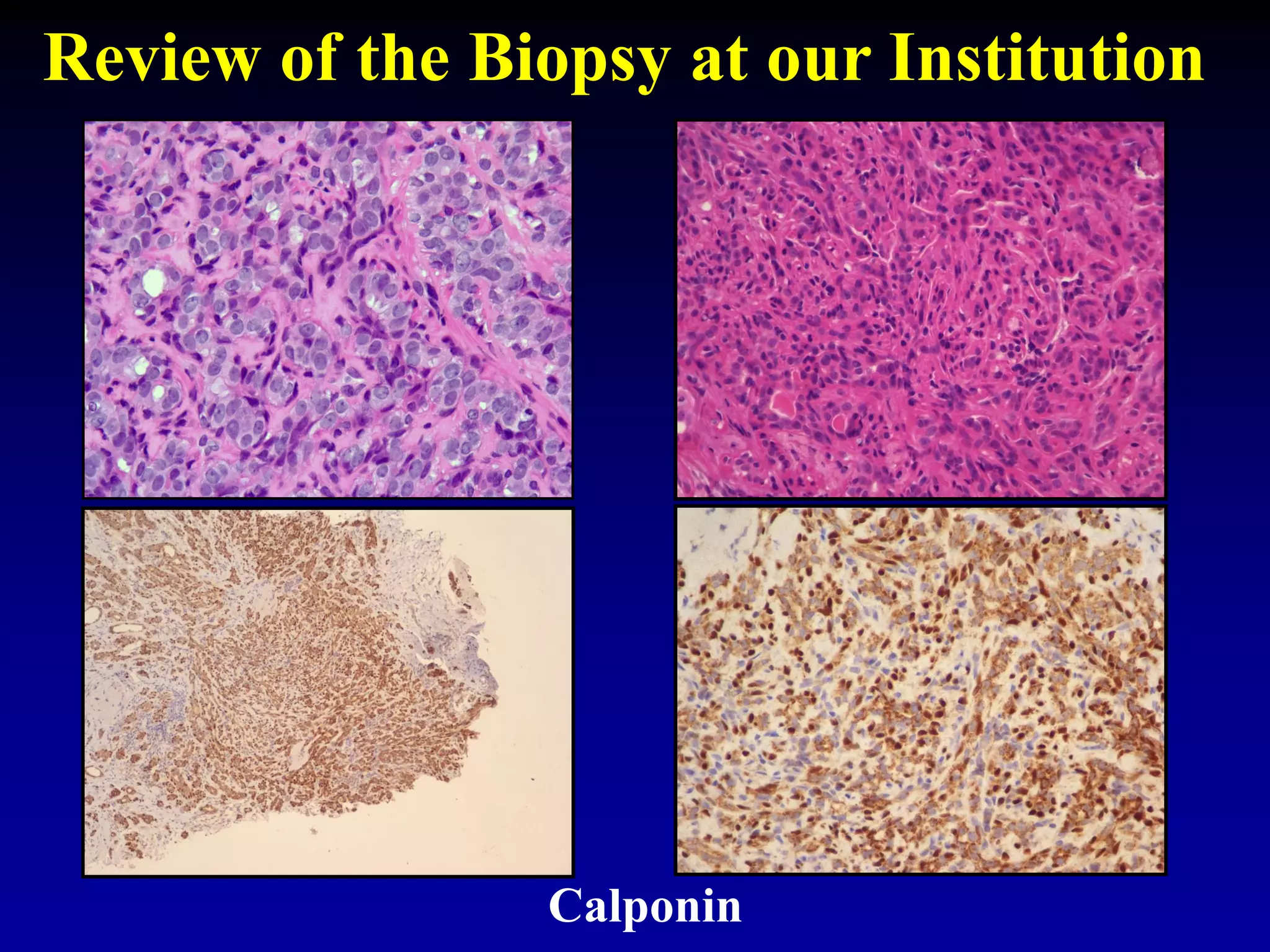
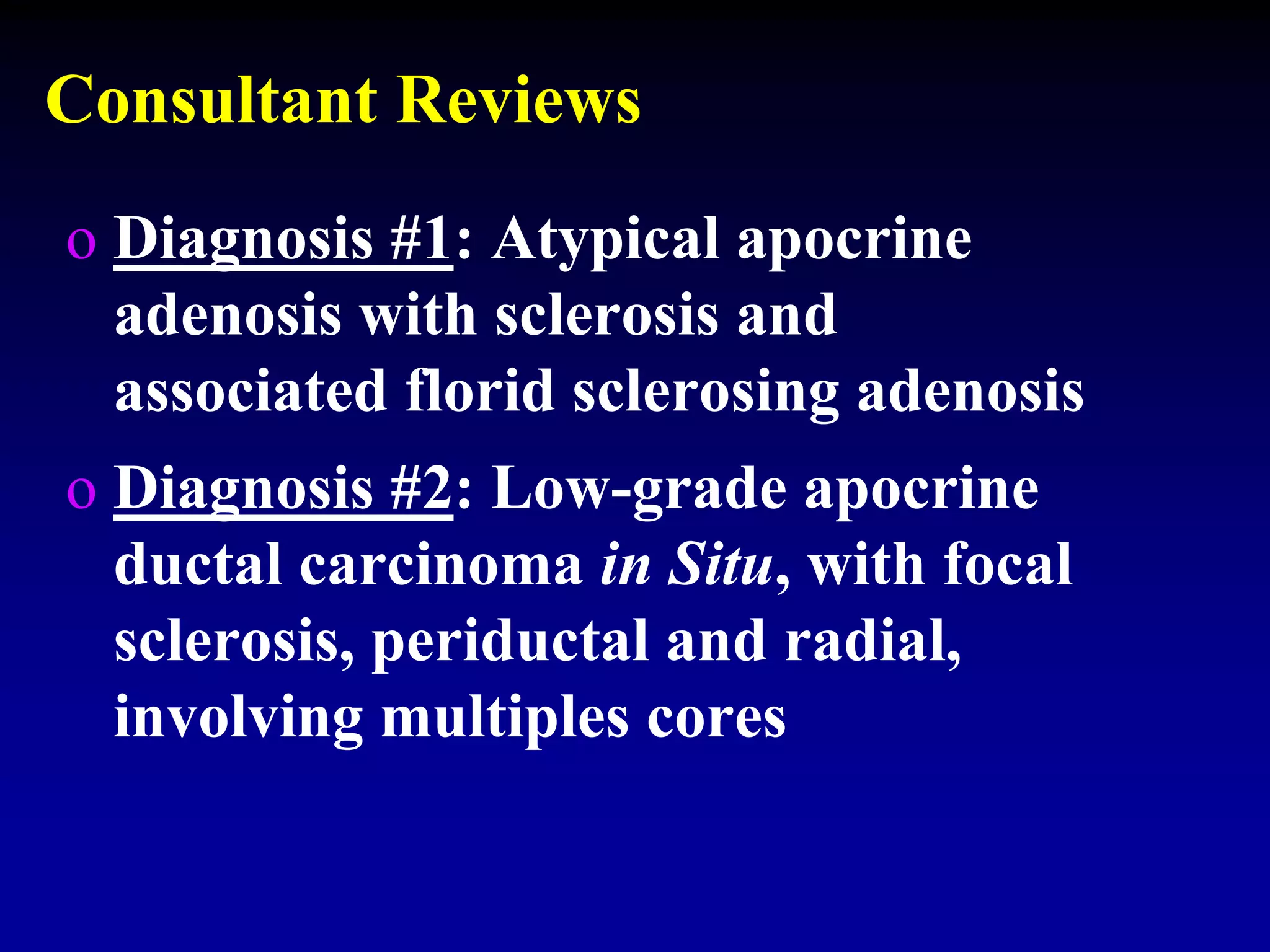
- Errors can occur so quality assurance like second reviews are important. A case was discussed where a diagnosis changed from invasive cancer to benign through further review, avoiding unnecessary mastectomy.