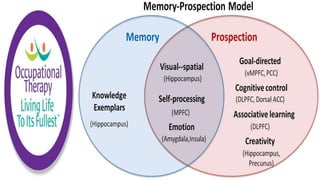
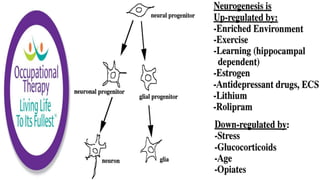
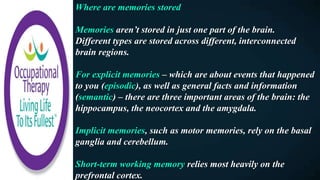
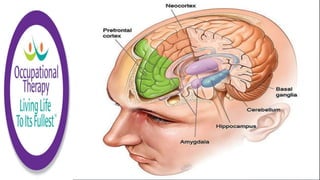
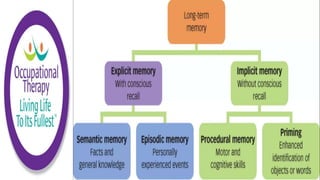
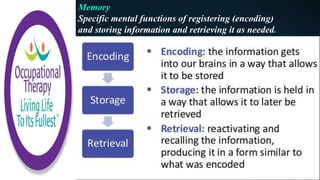
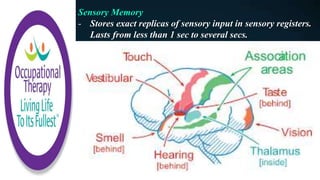
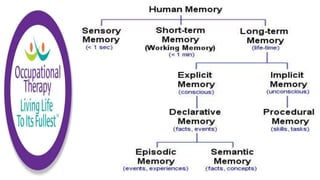
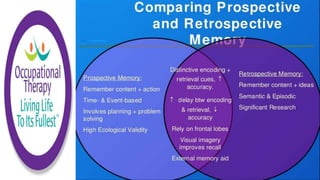
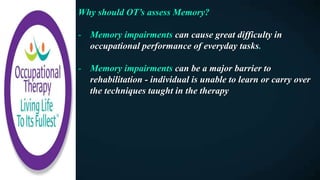
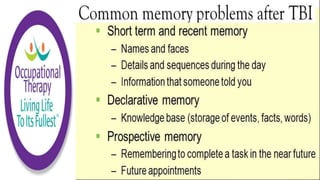
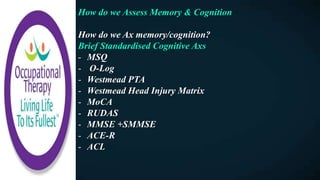
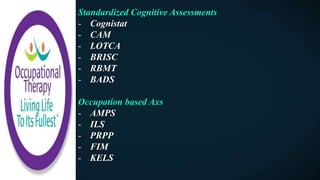
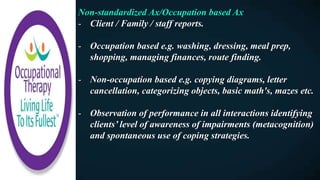
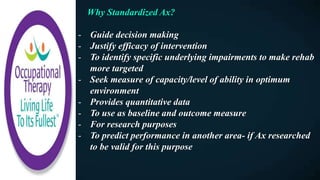
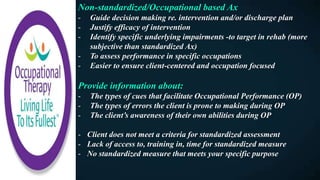
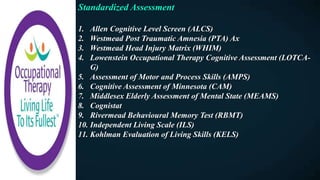
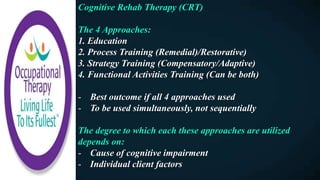
This document discusses how memories are formed and stored in the brain. It explains that memories are formed through synaptic plasticity, which refers to changes in the strength of connections between neurons. These connections are made stronger or weaker based on past activation patterns. Three key areas involved in memory are the hippocampus, which forms episodic memories; the amygdala, which attaches emotional significance; and the neocortex, where memories may be consolidated over time. Different memory systems rely on different brain regions, such as the basal ganglia and cerebellum for implicit memories, and the prefrontal cortex for working memory. The document also outlines how occupational therapists assess memory through standardized tests and occupation-based evaluations.