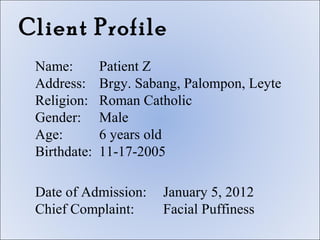
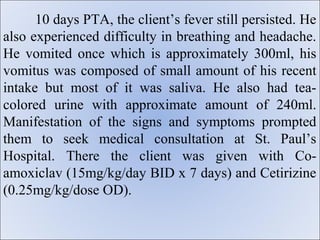
The document outlines the objectives and introduction for a case study on a 6-year-old male patient admitted with facial puffiness. The patient's history notes a recent illness with fever, difficulty breathing, vomiting, and tea-colored urine. Laboratory results showed a urinary tract infection and abnormalities. The patient's family, medical, developmental, and social histories are provided. The document establishes the background for analyzing the patient's condition and developing a nursing care plan.