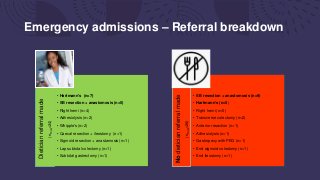
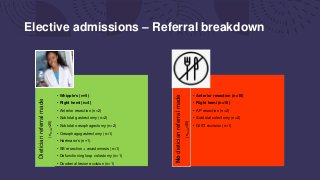
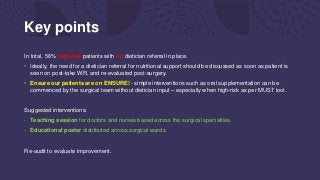
This document summarizes an audit of postoperative nutritional management of 100 emergency and elective surgical patients at UHNM. For emergency patients, 48% received a dietician referral but 56% of high-risk patients did not. Elective patients had a lower referral rate of 40%. Patients without referrals had more complications. The discussion notes most UK hospitals struggle with identifying and managing malnutrition perioperatively due to various organizational challenges. The key points recommend discussing nutritional needs earlier, ensuring oral supplementation, and staff education to improve postoperative nutritional care.