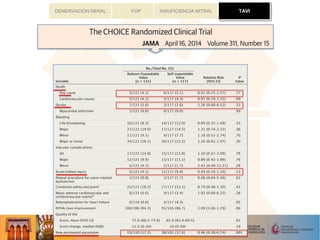
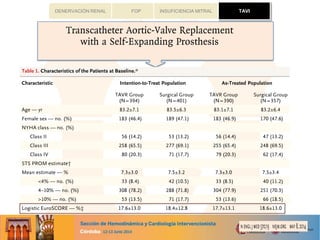
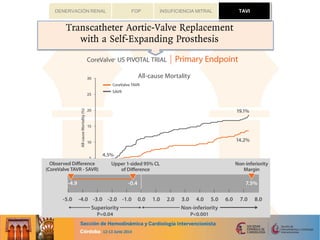
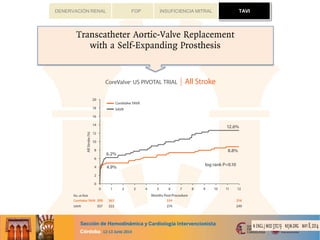
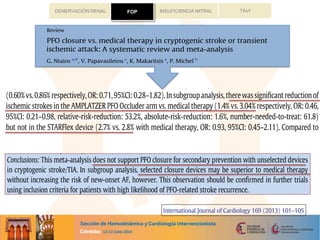
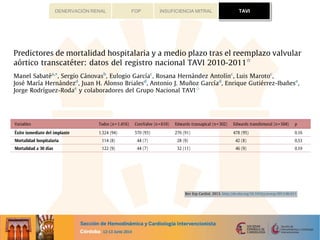
This document summarizes the results of the German Aortic Valve Registry (GARY) which collected data on 13,860 patients undergoing either conventional surgery or catheter-based procedures for aortic valve disease in 2011. The registry included data on 6,523 patients who underwent conventional aortic valve replacement without coronary bypass surgery (AVR), 3,464 who underwent AVR with coronary bypass surgery (AVR+CABG), 2,695 who underwent transvascular catheter-based aortic valve implantation (TAVI), and 1,181 who underwent transapical TAVI. Patients who underwent catheter-based procedures were significantly older and had higher risk profiles. The in-hospital stroke rates were low across all groups. In-


![TAVIFOP INSUFICIENCIA MITRALDENERVACIÓN RENAL
...........................................................................................................................................................
...........................................................................................................................................................
sPapoutsis,Steffen Schneider,Armin W elz,and Friedrich W .Mohr,for the
utive Board
y, Medical Clinic I,Kerckhoff Heart and Thorax Center, University of Giessen, Benekestrasse. 2-8, Bad Nauheim 61231,Germany
sed 5 August 2013;accepted 22 August 2013
Aorticstenosisisafrequent valvular diseaseespeciallyinelderlypatients.Catheter-basedvalveimplantationhasemerged
asavaluabletreatment approachfor thesepatientsbeingeither at veryhighriskfor conventional surgeryor evendeemed
inoperable.TheGermanAorticValveRegistry(GARY) providesdataonconventional andcatheter-based aorticproce-
dureson an all-comersbasis.
A total of13860consecutivepatientsundergoingrepair for aorticvalvedisease[conventional surgeryandtransvascular
(TV) or transapical (TA) catheter-basedtechniques] havebeenenrolledinthisregistryduring2011andbaseline,proced-
ural,andoutcomedatahavebeenacquired.Theregistrysummarizestheresultsof6523conventional aorticvalverepla-
cementswithout (AVR)and3464withconcomitant coronarybypasssurgery(AVR+ CABG)aswellas2695TVAVIand
1181 TA interventions(TA AVI).Patientsundergoingcatheter-based techniquesweresignificantly older andhadhigher
risk profiles.Thestrokeratewaslow inall groupswith1.3%(AVR),1.9%(AVR+ CABG),1.7%(TVAVI),and 2.3%(TA
AVI).Thein-hospital mortality was2.1%(AVR) and4.5%(AVR+ CABG) for patientsundergoingconventional surgery,
and 5.1%(TVAVI) and AVI 7.7%(TA AVI).
Thein-hospital outcomeresultsof thisregistryshow that conventional surgery yieldsexcellent resultsinall risk groups
and that catheter-based aortic valve replacements is an alternative to conventional surgery in high risk and elderly
patients.
------------------------------------------------------------------------------------------------------------------------------------
Aortic stenosis † Surgery † Catheter-based valvereplacement † GARY
.....................................................................................................................................................................................
.....................................................................................................................................................................................
CLIN ICAL RESEARCH
The German Aortic Valve Registry
(GARY): in-hospital outcome
Christian W . Hamm*, Helge Mo¨llmann, David Holzhey, Andreas Beckmann,
Christof Veit, Hans-Reiner Figulla, J. Cremer, Karl-Heinz Kuck, Ru¨diger Lange,
Ralf Zahn, Stefan Sack, Gerhard Schuler, Thomas W alther, Friedhelm Beyersdorf,
Michael Bo¨hm, Gerd Heusch, Anne-Kathrin Funkat, Thomas Meinertz, Till Neumann,
KonstantinosPapoutsis, Steffen Schneider, Armin W elz, and Friedrich W . Mohr, for the
GARY-Executive Board
Department of Cardiology, Medical Clinic I, Kerckhoff Heart and Thorax Center, University of Giessen, Benekestrasse. 2-8, Bad Nauheim 61231, Germany
Received 24 May2013; revised 5 August 2013; accepted 22 August 2013
Back gr ound Aorticstenosisisafrequent valvular diseaseespeciallyinelderlypatients.Catheter-basedvalveimplantationhasemerged
asavaluabletreatment approachfor thesepatientsbeingeither at veryhighrisk for conventional surgeryor evendeemed
inoperable.TheGerman Aortic ValveRegistry (GARY) providesdataonconventional and catheter-based aortic proce-
dureson an all-comers basis.
Met hods and
r esult s
A total of 13 860consecutive patientsundergoingrepair for aortic valvedisease[conventional surgery and transvascular
(TV) or transapical (TA) catheter-based techniques] havebeenenrolledinthisregistryduring2011andbaseline,proced-
ural,and outcomedatahavebeen acquired.Theregistry summarizestheresultsof 6523 conventional aortic valverepla-
cementswithout (AVR) and3464withconcomitant coronarybypasssurgery(AVR+ CABG) aswell as2695TVAVIand
1181 TA interventions(TA AVI). Patientsundergoingcatheter-based techniquesweresignificantly older and had higher
risk profiles. The strokeratewaslow in all groupswith 1.3%(AVR), 1.9%(AVR+ CABG), 1.7%(TVAVI), and 2.3%(TA
AVI).Thein-hospital mortality was2.1%(AVR) and 4.5%(AVR+ CABG) for patientsundergoingconventional surgery,
and 5.1%(TVAVI) and AVI 7.7%(TA AVI).
Conclusion The in-hospital outcome resultsof thisregistry show that conventional surgery yieldsexcellent resultsin all risk groups
and that catheter-based aortic valve replacements is an alternative to conventional surgery in high risk and elderly
patients.
-----------------------------------------------------------------------------------------------------------------------------------------------------------
Keywor ds Aortic stenosis † Surgery † Catheter-based valve replacement † GARY
Introduction
Aortic stenosis is the most frequent type of valvular heart disease
in the Western Countries and presents mostly in an advanced age
as a calcific form. The prognosis is poor once the patient becomes
symptomatic. Surgical valve replacement isthe established standard
management, which alleviates symptoms and improves survival.1
Valvuloplasty of the stenosed valve hasbeen over many yearsapal-
liative option for the short term for highly selected, inoperable
patients. Recently, catheter-based valve implantations have
become an alternative for selected, particularly elderly
patients.2–4
Smaller, randomized studies confirmed acceptable
outcomesinhighriskandinoperablepatients5,6
for thetransvascu-
lar (TV) as well asthe transapical (TA) approach when compared
European Heart Journal
doi:10.1093/eurheartj/eht381
atBibliotecaVirtualdelSistemaSanitarioPúblicodeAndalucÃ-aonMarch17,2014http://eurheartj.oxfordjournals.org/Downloadedfrom
TAVI
CLINICAL RESEEuropeanHeart Journal
doi:10.1093/eurheartj/eht381
European Heart Journal Advance Access published September 10, 2013](https://image.slidesharecdn.com/novedadesschi2014josemariahernandez-140625072853-phpapp02/85/Cardiopatia-Estructural-Dr-Jose-Maria-Hernandez-15-320.jpg)
![TAVIFOP INSUFICIENCIA MITRALDENERVACIÓN RENAL
.....................................................................................................................................................................................
.....................................................................................................................................................................................
The German Aortic Valve Registry
(GARY): in-hospital outcome
Christian W . Hamm*, Helge Mo¨llmann, David Holzhey, AndreasBeckmann,
Christof Veit, Hans-Reiner Figulla, J. Cremer, Karl-Heinz Kuck, Ru¨diger Lange,
Ralf Zahn, Stefan Sack, Gerhard Schuler, ThomasW alther, Friedhelm Beyersdorf,
Michael Bo¨hm, Gerd Heusch, Anne-Kathrin Funkat, ThomasMeinertz, Till Neumann,
KonstantinosPapoutsis,Steffen Schneider,Armin W elz,and Friedrich W .Mohr,for the
GARY-Executive Board
Department of Cardiology, Medical Clinic I, Kerckhoff Heart and Thorax Center, University of Giessen, Benekestrasse. 2-8, Bad Nauheim 61231,Germany
Received24 May2013;revised 5 August 2013;accepted 22 August 2013
Background Aorticstenosisisafrequent valvular diseaseespeciallyinelderlypatients.Catheter-basedvalveimplantationhasemerged
asavaluabletreatment approachfor thesepatientsbeingeither at veryhighriskfor conventional surgeryor evendeemed
inoperable.TheGermanAorticValveRegistry(GARY) providesdataonconventional andcatheter-based aorticproce-
dureson an all-comersbasis.
Met hods and
result s
A total of13860consecutivepatientsundergoingrepair for aorticvalvedisease[conventional surgeryandtransvascular
(TV) or transapical (TA) catheter-based techniques] havebeenenrolledinthisregistryduring2011andbaseline,proced-
ural,andoutcomedatahavebeenacquired.Theregistrysummarizestheresultsof 6523conventional aorticvalverepla-
cementswithout (AVR) and3464withconcomitant coronarybypasssurgery(AVR+ CABG) aswellas2695TVAVIand
1181TA interventions(TA AVI).Patientsundergoingcatheter-based techniquesweresignificantly older and had higher
risk profiles.Thestrokeratewaslow inall groupswith 1.3%(AVR),1.9%(AVR+ CABG),1.7%(TVAVI),and 2.3%(TA
AVI).Thein-hospital mortality was2.1%(AVR) and4.5%(AVR+ CABG) for patientsundergoingconventional surgery,
and 5.1%(TVAVI) and AVI 7.7%(TA AVI).
Conclusion Thein-hospital outcomeresultsof thisregistry show that conventional surgery yieldsexcellent resultsin all risk groups
and that catheter-based aortic valve replacements is an alternative to conventional surgery in high risk and elderly
patients.
-----------------------------------------------------------------------------------------------------------------------------------------------------------
Keywords Aortic stenosis † Surgery † Catheter-based valvereplacement † GARY
Introduction
Aortic stenosis is the most frequent type of valvular heart disease
in the Western Countries and presents mostly in an advanced age
Valvuloplasty of the stenosed valvehasbeen over many yearsapal-
liative option for the short term for highly selected, inoperable
patients. Recently, catheter-based valve implantations have
become an alternative for selected, particularly elderly
European Heart Journal
doi:10.1093/eurheartj/eht381
atBibliotecaVirtualdelSistemaSanitarioPúblicodeAndalucÃ-aonMarch17,2014http://eurheartj.oxfordjournals.org/Downloadedfrom
TAVI
CLINICAL RESEAEuropeanHeart Journal
doi:10.1093/eurheartj/eht381
European Heart Journal Advance Access published September 10, 2013](https://image.slidesharecdn.com/novedadesschi2014josemariahernandez-140625072853-phpapp02/85/Cardiopatia-Estructural-Dr-Jose-Maria-Hernandez-16-320.jpg)
![TAVIFOP INSUFICIENCIA MITRALDENERVACIÓN RENAL
.....................................................................................................................................................................................
.....................................................................................................................................................................................
CLIN ICA L RESA RCH
TAVI
Advanced chronic kidney disease in pat ient s
undergoing t ranscat het er aort ic valve
implant at ion: insight s on clinical out comes and
prognost ic markersfrom a large cohort of pat ient s
Ricar do A llende1†, John G. W ebb2, A nt onio J. Munoz-Gar cia3, Pet er de Jaeger e4,
Cor r ado T am bur ino5, A nt onio E. Dager 6, A sim Cheem a7, Vicenc¸ Ser r a8,
Ignacio A m at -Sant os9, Jam es L. Velianou10, Mar co Bar bant i2, Danny Dvir 2,
Juan H . A lonso-Br iales3, Rut ger -Jan N uis4, Elham ula Faqir i 4, Sebast iano Im m e5,
Luis Miguel Benit ez6, A ngela Mar ia Cucalon6, H at im A l Lawat i7,
Br uno Gar cia del Blanco8, Javier Lopez9, Madhu K. N at ar ajan10,
Rober t DeLar ochellie`r e1, Mar ina U r ena1, H enr ique B. Ribeir o1, Er ic Dum ont 1,
Luis N om bela-Fr anco 1†, and Josep Rode´s-Cabau1*
1
Quebec Heart and LungInstitute, Laval University, Quebec city,QC,Canada; 2
St Paul’sHospital,University of British Columbia, Vancouver,BC,Canada; 3
Hospital Universitario Virgen de
la Victoria, Malaga, Spain; 4
Thoraxcenter-Erasmus MC, Rotterdam, The Netherlands; 5
Ferrarotto Hospital, University of Catania, Catania, Italy; 6
Angiografia de Occidente S.A., Cali,
Colombia; 7
St-Michael’sHospital, Toronto, ON, Canada; 8
Hospital General Universitari Vall d’Hebron, Barcelona, Spain; 9
Hospital Clinico Universitario de Valladolid, Valladolid, Spain;
and 10
Hamilton General Hospital, Hamilton, ON, Canada
Received 11 August 2013; revised 9 February 2014; accepted 3 April 2014
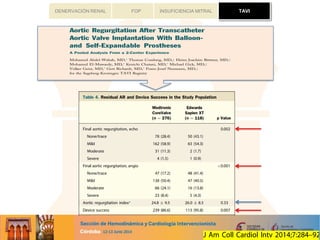
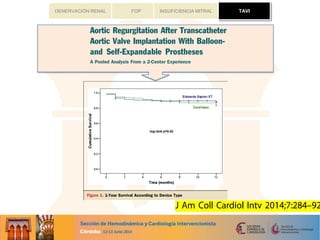
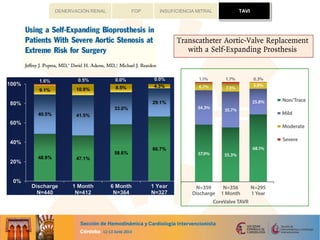
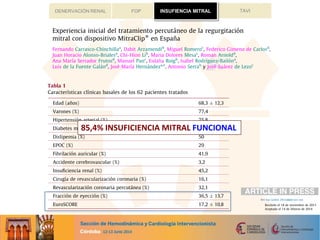
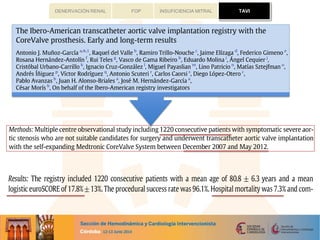
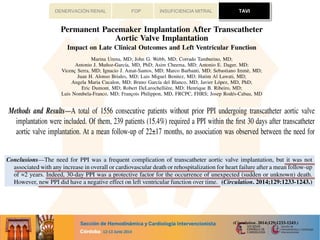
A im Theaimofthisstudywasto determinetheeffectsofadvancedchronickidneydisease(CKD) onearlyandlateoutcomesafter
transcatheter aortic valve implantation (TAVI), and to evaluate the predictive factorsof poorer outcomesin such patients.
M et hods
and r esult s
This was a multicentre study including a total of 2075 consecutive patients who had undergone TAVI. Patients were
grouped according the estimated glomerular filtration rate as follows: CKD stage 1-2 (≥ 60 mL/min/1.73 m2
;
n ¼ 950), stage 3 (30–59 mL/min/1.73 m2
; n ¼ 924), stage 4 (15–29 mL/min/1.73 m2
; n ¼ 134) and stage 5 (, 15 mL/
min/1.73 m2
or dialysis; n ¼ 67). Clinical outcomes were evaluated at 30-days and at follow-up (median of 15 [6–29]
months) and defined according to the VARC criteria. Advanced CKD (stage 4–5) was an independent predictor of
30-day major/life-thr eatening bleeding (P¼ 0.001) and mortality (P¼ 0.027), and late overall, cardiovascular and non-
cardiovascular mortality (P, 0.01 for all).Pre-existingatrial fibrillation (HR:2.29,95%CI:1.47–3.58,P¼ 0.001) and dia-
lysistherapy (HR: 1.86, 95%CI: 1.17–2.97, P¼ 0.009) were the predictorsof mortality in advanced CKD patients, with a
mortality rate ashigh as71%at 1-year follow-up in those patientswith these 2 factors. Advanced CKD patientswho had
survived at 1-year follow-up exhibited both asignificant improvement in NYHA class(P, 0.001) and no deterioration in
valve hemodynamics (P¼ NSfor changes in mean gradient and valve area over time).
Conclusions Advanced CKD wasassociated withahigher rateof earlyand latemortalityand bleedingeventsfollowingTAVI,withAFand
dialysistherapydeterminingahigher risk inthesepatients.Themortality rateof patientswith both factorswasunacceptably
high and thisshould be taken into account in the clinical decision-makingprocessin thischallenginggroup of patients.
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
K eyw o r ds Chronic kidney disease † Dialysis † Transcatheter aortic valve implantation † Atrial fibrillation
* Corresponding author. Tel: + 1 4186568711, Fax:+ 1 4186564544, Email: josep.rodes@criucpq.ulaval.ca
†
R.A. and L.N.-F. have equally contributed to this work.
Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2014. For permissions please email: journals.per missions@oup.com.
European Heart Journal
doi:10.1093/eurheartj/ehu175
atBibliotecaVirtualdelSistemaSanitarioPúblicodeAndalucÃ-aonJune4,2014http://eurheartj.oxfordjournals.org/Downloadedfrom
...........................................................................................................................................................
...........................................................................................................................................................
arochellie`re1, Marina Urena1, Henrique B. Ribeiro1, Eric Dumont1,
la-Franco1†
, and Josep Rode´s-Cabau1*
stitute,Laval University,Quebeccity,QC,Canada;2
St Paul’sHospital,UniversityofBritishColumbia,Vancouver,BC,Canada;3
Hospital Universitario Virgende
Thoraxcenter-Erasmus MC, Rotterdam, The Netherlands;5
Ferrarotto Hospital,University of Catania, Catania, Italy; 6
Angiografiade Occidente S.A., Cali,
ospital, Toronto, ON,Canada; 8
Hospital General Universitari Vall d’Hebron, Barcelona, Spain; 9
Hospital Clinico Universitario deValladolid, Valladolid, Spain;
ospital, Hamilton, ON, Canada
evised 9 February2014;accepted 3 April 2014
Theaimofthisstudywastodeterminetheeffectsofadvancedchronickidneydisease(CKD)onearlyandlateoutcomesafter
transcatheter aorticvalveimplantation(TAVI),andto evaluatethepredictivefactorsof poorer outcomesinsuchpatients.
This was a multicentre study including a total of 2075 consecutive patients who had undergone TAVI. Patients were
grouped according the estimated glomerular filtration rate as follows: CKD stage 1-2 (≥ 60 mL/min/1.73 m2
;
n ¼ 950), stage 3 (30–59 mL/min/1.73 m2
; n¼ 924), stage 4 (15–29 mL/min/1.73 m2
;n¼ 134) and stage 5 (, 15 mL/
min/1.73 m2
or dialysis; n ¼ 67). Clinical outcomes were evaluated at 30-daysand at follow-up (median of 15 [6–29]
months) and defined according to the VARC criteria. Advanced CKD (stage 4–5) was an independent predictor of
30-day major/life-threateningbleeding(P¼ 0.001) and mortality (P¼ 0.027), and late overall, cardiovascular and non-
cardiovascular mortality(P, 0.01for all).Pre-existingatrial fibrillation(HR:2.29,95%CI:1.47–3.58,P¼ 0.001) anddia-
lysistherapy(HR:1.86,95%CI:1.17–2.97,P¼ 0.009) werethepredictorsofmortalityinadvanced CKD patients,witha
mortality rateashighas71%at 1-year follow-upinthosepatientswiththese2factors.Advanced CKD patientswho had
survivedat 1-year follow-upexhibited bothasignificant improvement inNYHA class(P, 0.001) andno deteriorationin
valve hemodynamics (P¼ NSfor changesin mean gradient and valveareaover time).
AdvancedCKD wasassociatedwithahigher rateofearlyandlatemortalityandbleedingeventsfollowingTAVI,withAFand
dialysistherapydeterminingahigher riskinthesepatients.Themortalityrateofpatientswithbothfactorswasunacceptably
highand thisshould betaken into account in theclinical decision-makingprocessin thischallenginggroup of patients.
CLINICAL REuropean Heart Journal
doi:10.1093/eurheartj/ehu175
European Heart Journal Advance Access published May 5, 2014
CLINICAL REEuropeanHeart Journal
doi:10.1093/eurheartj/ehu175
European Heart Journal Advance Access published May 5, 2014
TAVI](https://image.slidesharecdn.com/novedadesschi2014josemariahernandez-140625072853-phpapp02/85/Cardiopatia-Estructural-Dr-Jose-Maria-Hernandez-18-320.jpg)