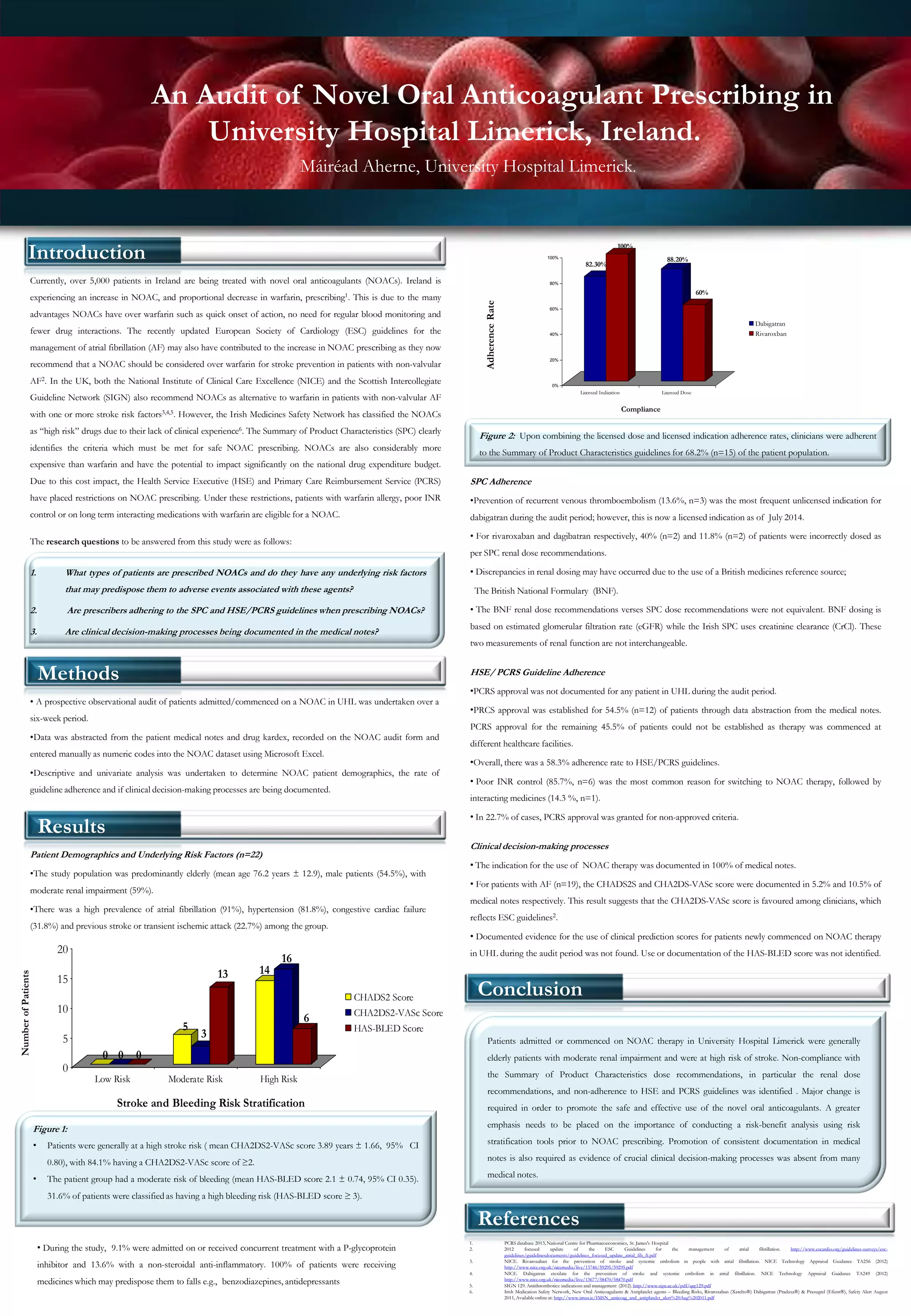
Patients prescribed novel oral anticoagulants (NOACs) in University Hospital Limerick were generally elderly with moderate risk of stroke and bleeding. Adherence to NOAC dosing guidelines was 68.2% and adherence to prescribing restrictions was 58.3%. Risk assessment scores were rarely documented and clinical decision making was not well documented. The study found significant non-compliance with NOAC dosing guidelines and prescribing restrictions, highlighting the need for improved risk assessment, documentation and guideline adherence when prescribing NOACs.