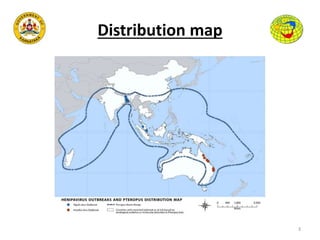
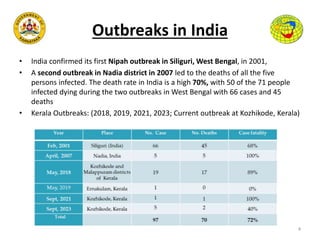
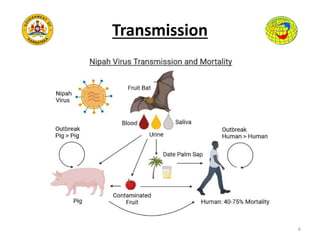
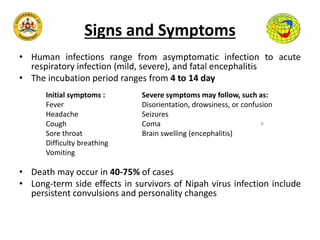
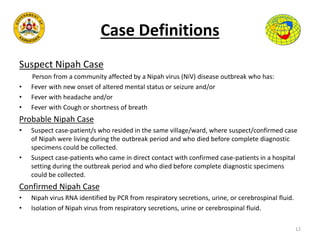
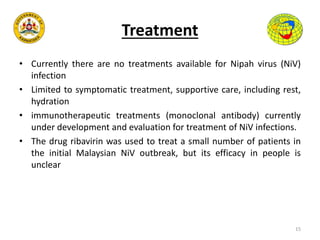
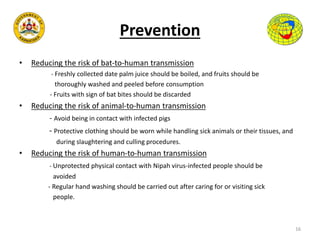
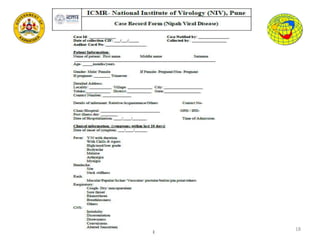
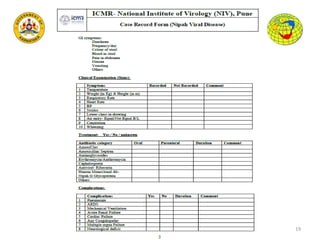
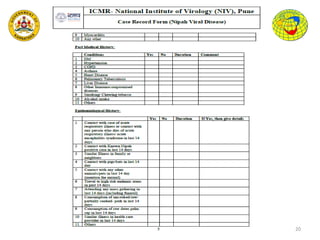
Nipah virus is an emerging zoonotic virus first identified in Malaysia in 1999. It is transmitted to humans from its natural reservoir, fruit bats of the Pteropodidae family. Outbreaks have occurred in India, Bangladesh and Malaysia. Symptoms in humans range from asymptomatic infection to acute respiratory distress and fatal encephalitis. There is no vaccine or treatment available, so prevention focuses on reducing human contact with infected bats or pigs. Surveillance and isolation of suspected cases is important to control outbreaks.