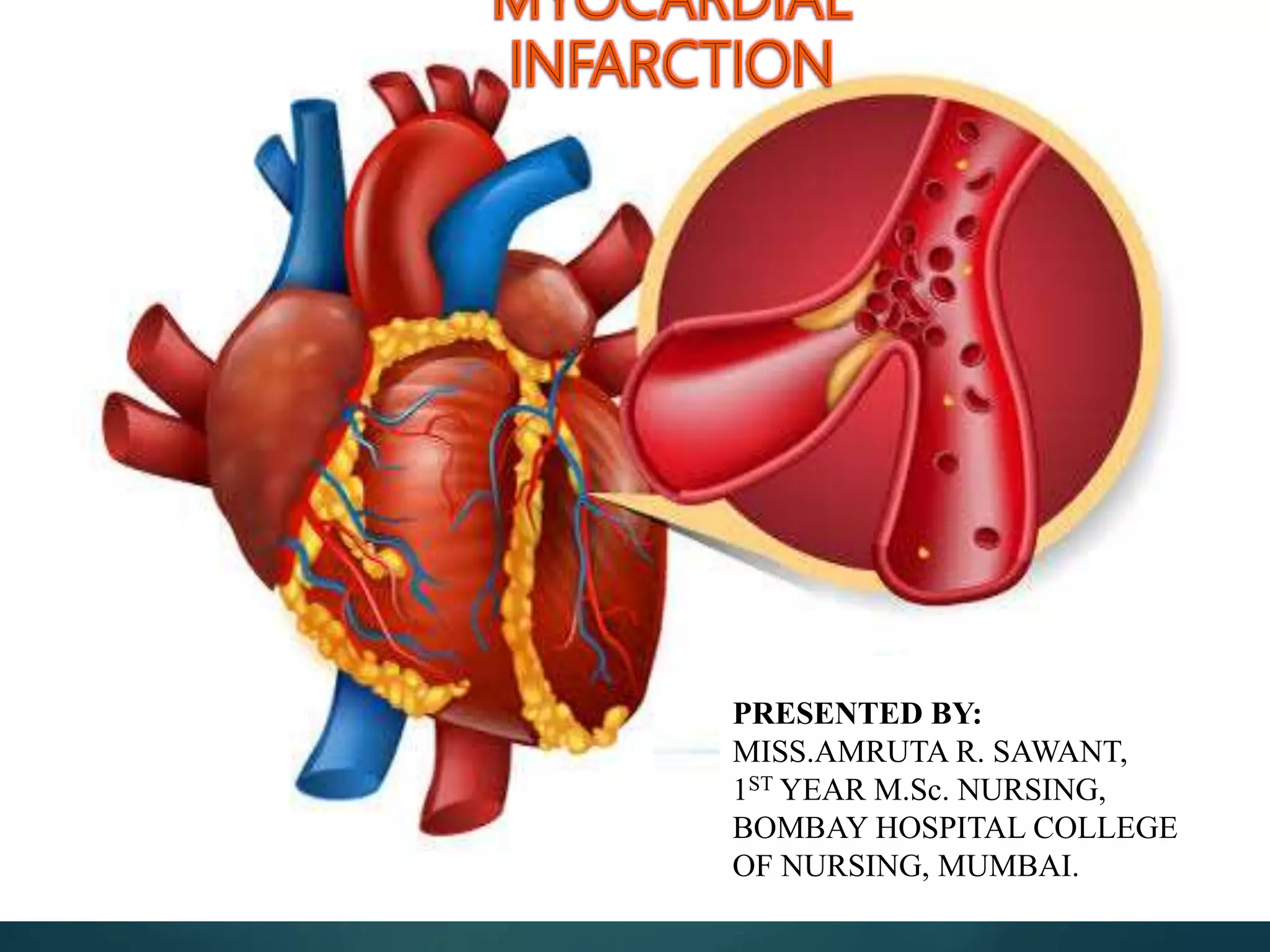
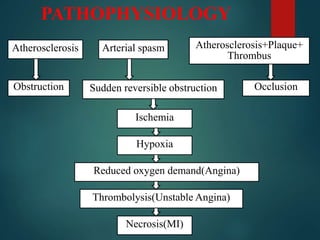
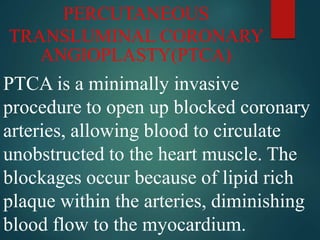
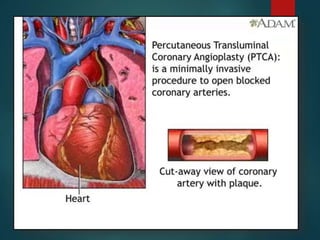
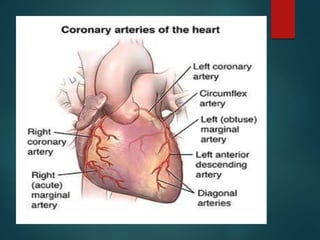
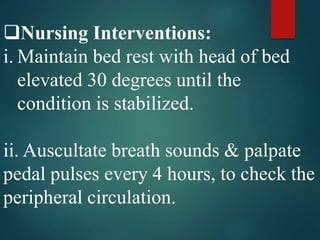
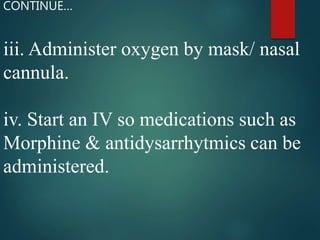
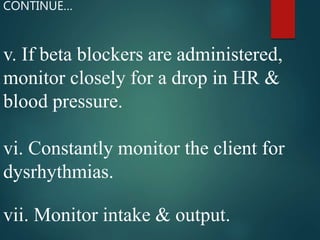
This document provides information about myocardial infarction (MI) or heart attack. It defines MI as occurring when blood flow to the heart is reduced or stopped, damaging heart muscle. MI is usually caused by a blockage in a coronary artery from atherosclerosis, clot, or embolism. The document then discusses the etiology, pathophysiology, clinical manifestations, diagnostic evaluations, pharmacological and surgical management, complications and nursing care for a patient experiencing an MI.