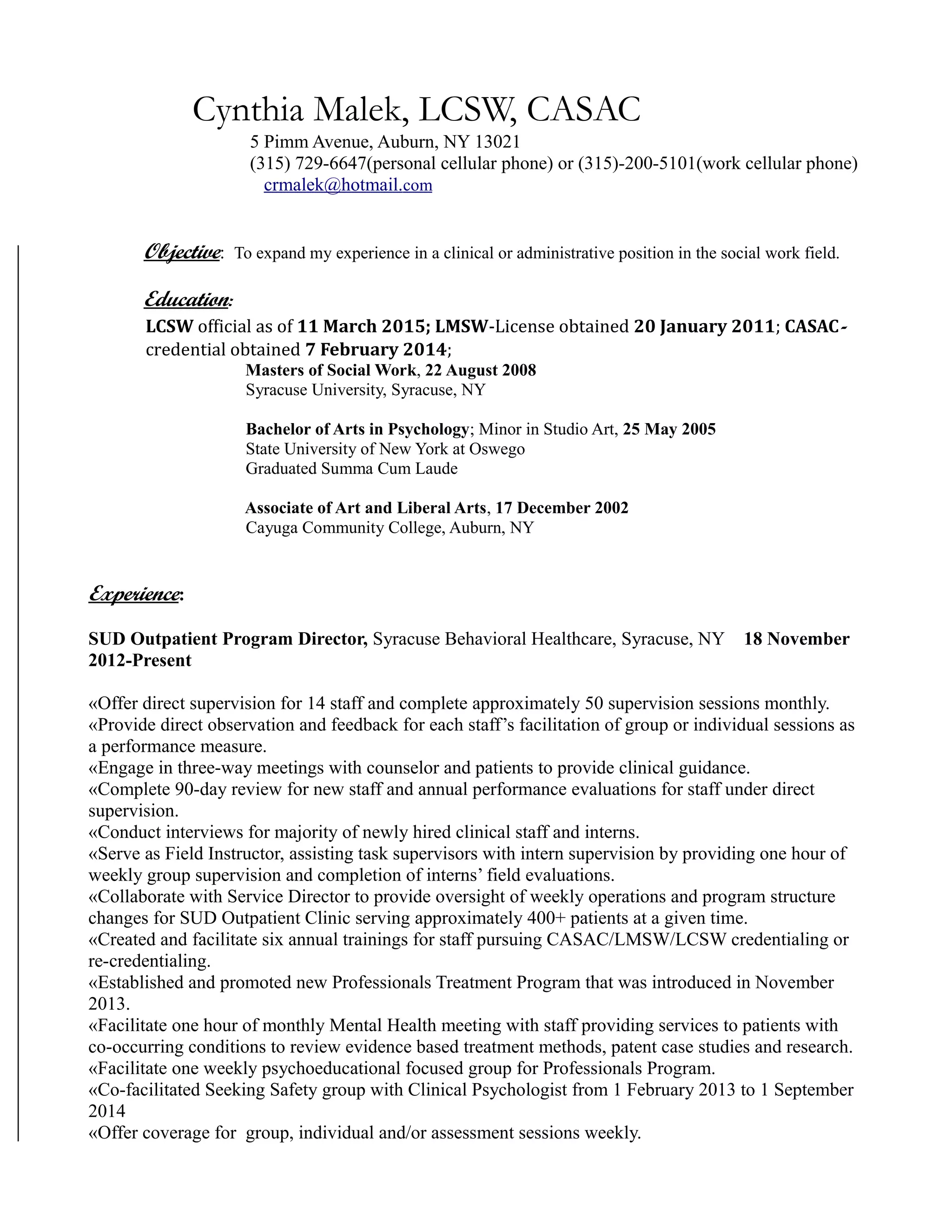
Cynthia Malek is a licensed clinical social worker and credentialed alcoholism and substance abuse counselor seeking to expand her experience in clinical or administrative social work positions. She has over 10 years of experience in substance use disorder treatment programs, including as the current director of an outpatient SUD program. Her experience includes clinical supervision, program administration, group and individual therapy, and working with clients with co-occurring disorders. She holds a Master's degree in social work and has additional credentials in counseling and substance abuse treatment.