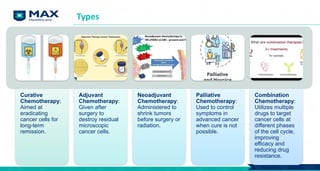
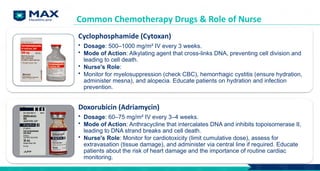
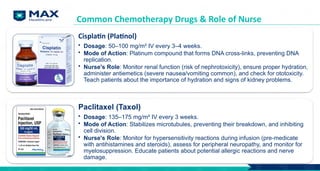
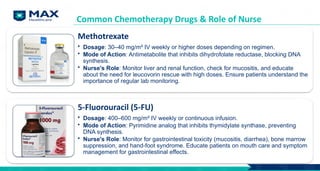
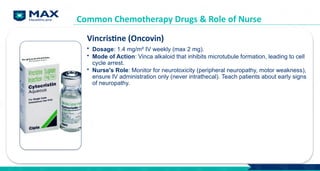
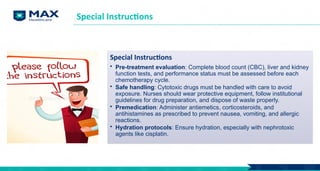
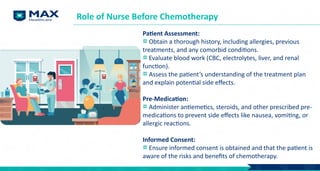
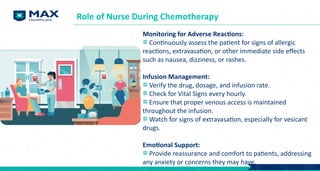
The document outlines key learning objectives for a module on cancer treatment modalities, focusing on imaging techniques and chemotherapy. It details the principles of MRI, radio nuclide imaging, and ultrasound in cancer care, along with chemotherapy types, indications, and common drugs used in treatment. The role of nurses in administering chemotherapy, managing side effects, and providing patient education and support is emphasized throughout.