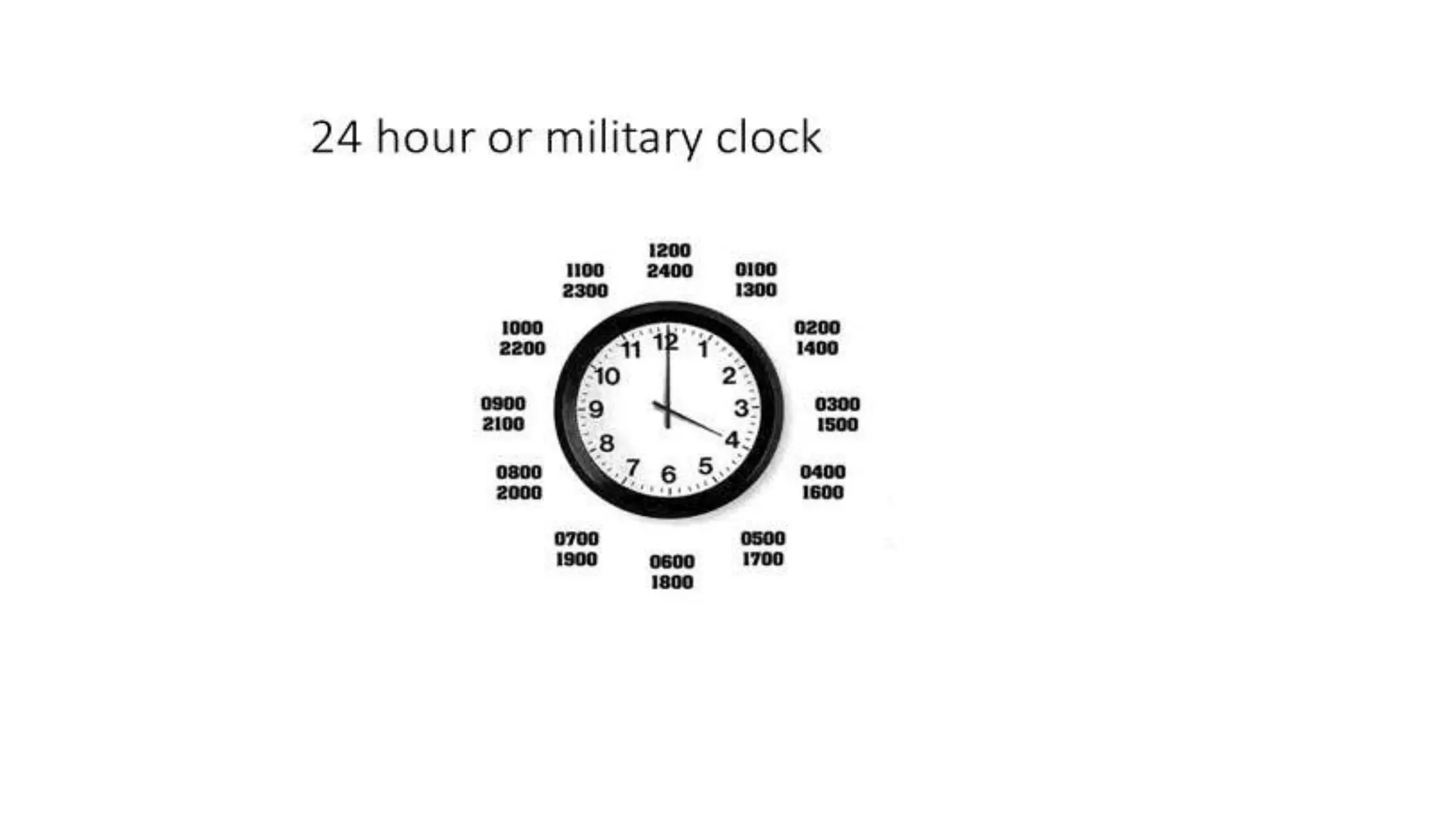
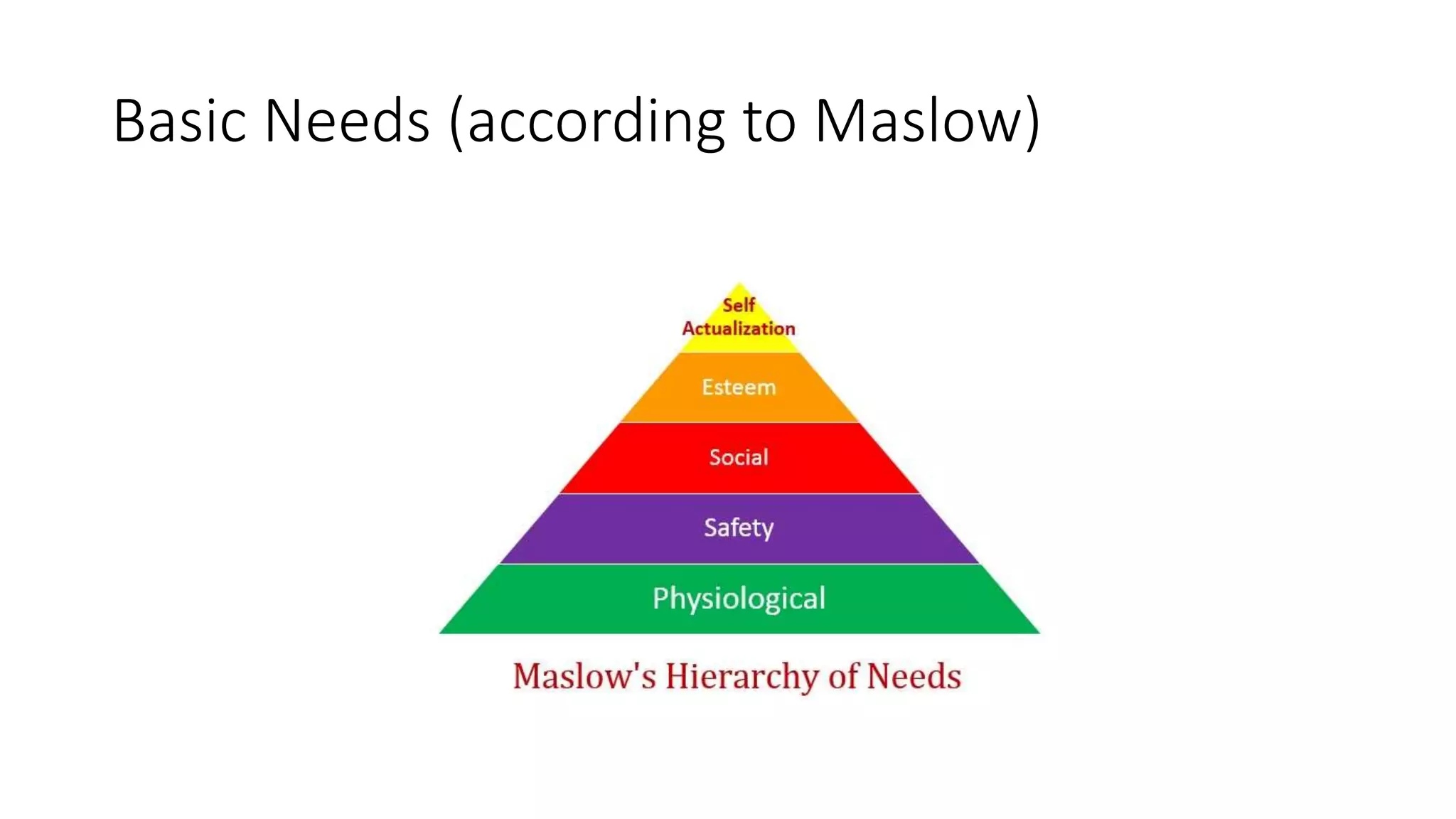
This document provides an overview of the Certified Nurse Aide program. It discusses long-term care settings like nursing homes, assisted living facilities, and skilled nursing facilities. It describes the types of illnesses served in these facilities and the interdisciplinary healthcare team. The nursing department structure and roles of nurses, nursing assistants, and other staff are defined. Key policies, procedures, and legal aspects of long-term care are summarized. Communication skills, stress management, and medical terminology relevant for nursing assistants are also covered.