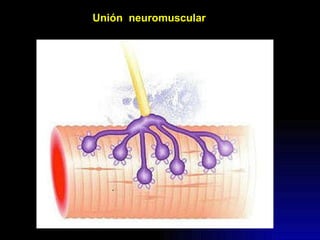
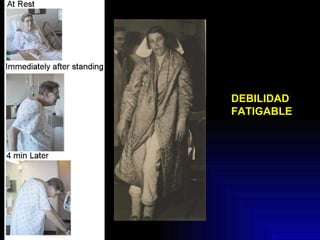
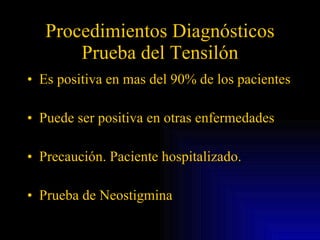
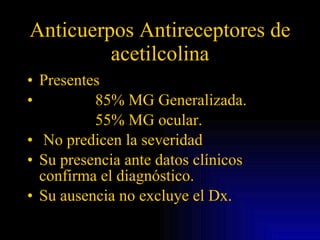
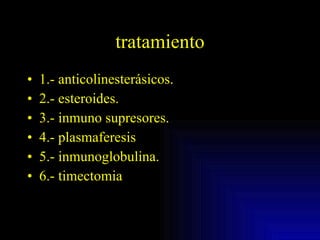
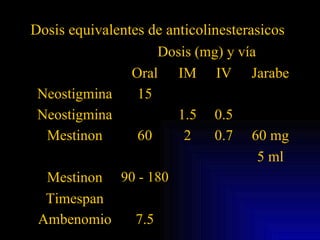
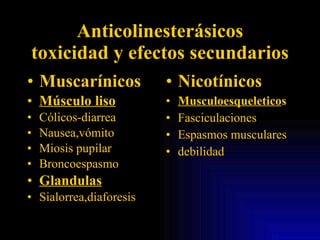
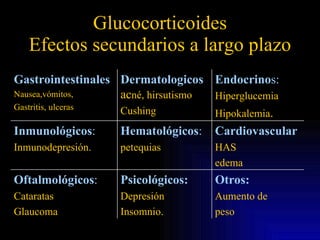
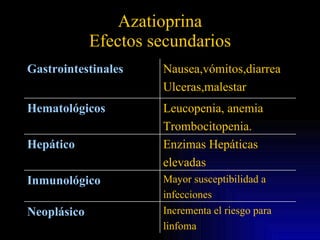
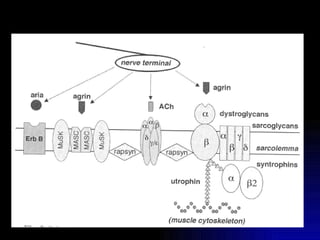
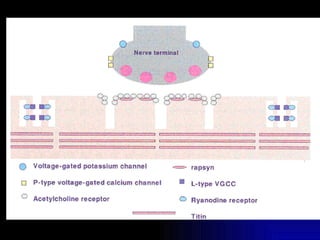
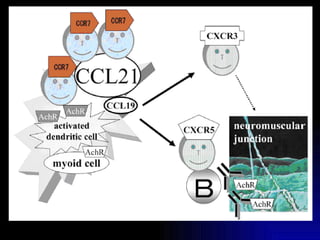
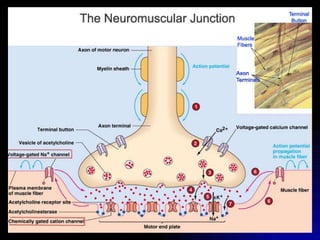
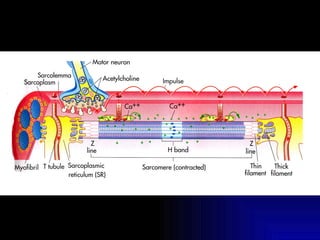
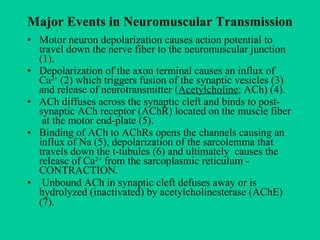
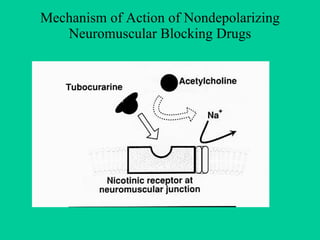
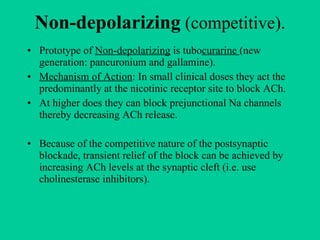
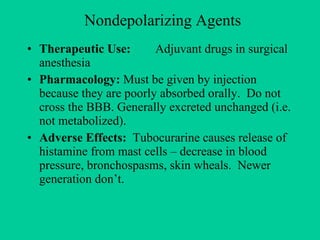
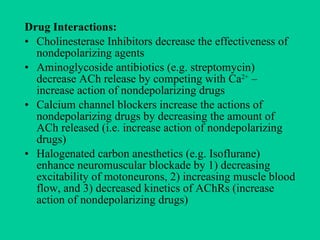
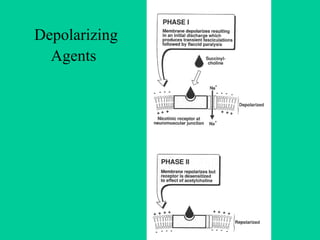
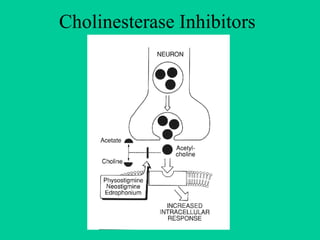
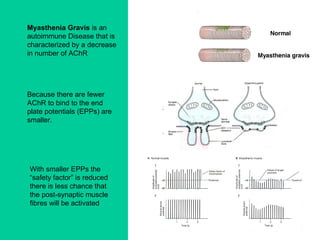
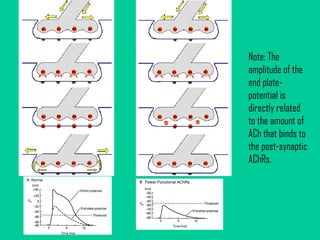
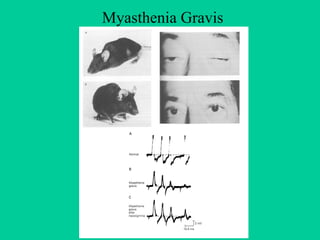
This document summarizes key events in neuromuscular transmission and discusses different types of neuromuscular blocking drugs used in surgery. It describes how non-depolarizing drugs like tubocurarine work competitively at nicotinic receptors to block acetylcholine, while depolarizing drugs like succinylcholine mimic acetylcholine's action. The document also discusses cholinesterase inhibitors and their use in treating myasthenia gravis by inhibiting breakdown of acetylcholine in the neuromuscular junction.