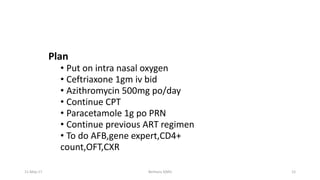
1) The document discusses the management of common opportunistic infections (OIs) and antiretroviral therapy (ART) failure in HIV patients.
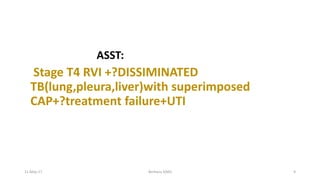
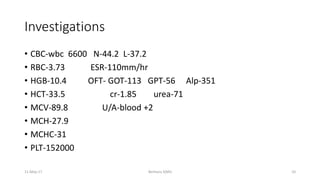
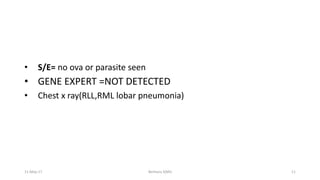
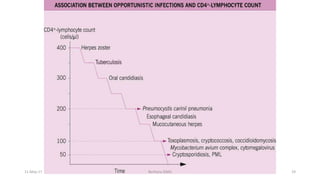
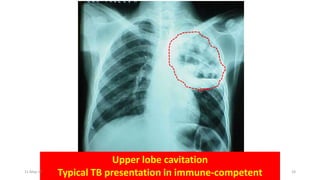
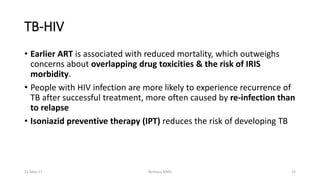
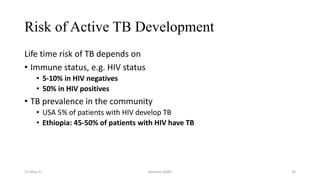
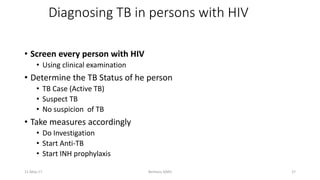
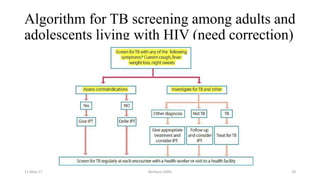
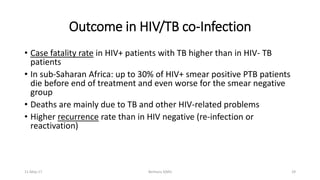
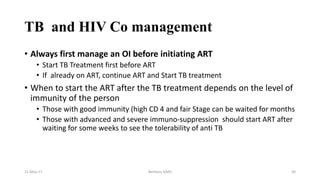
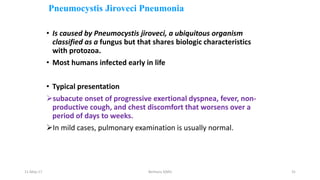
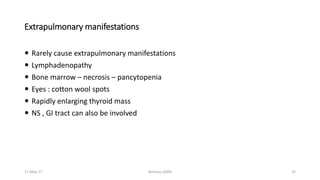
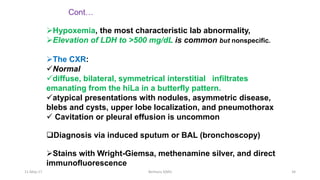
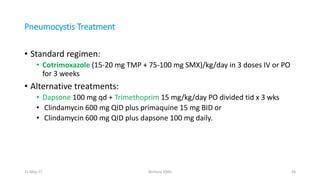
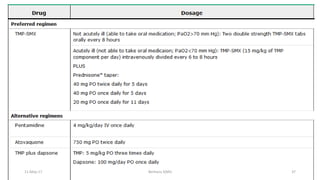
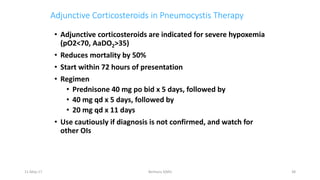
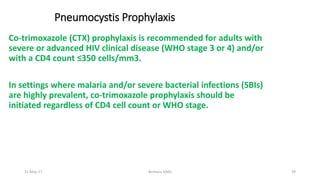
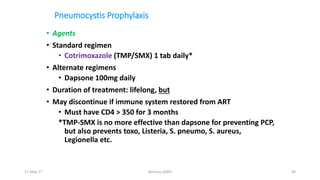
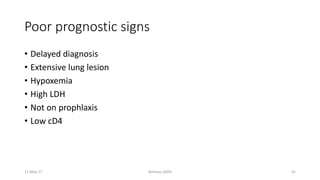
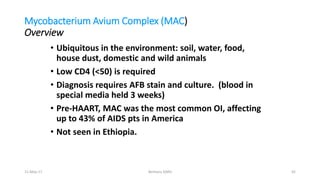
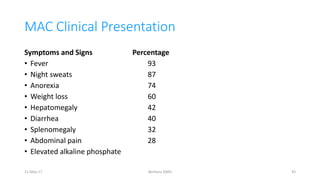
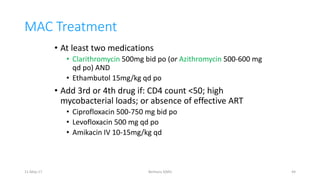
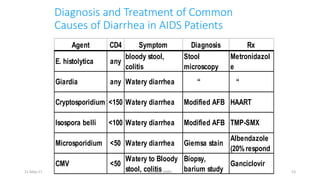
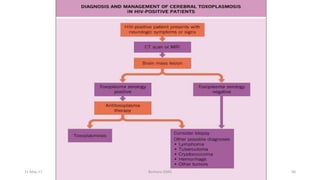
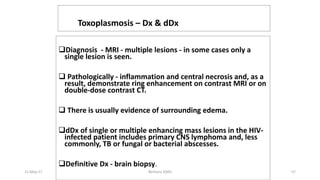
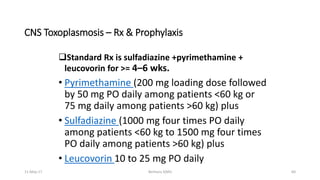
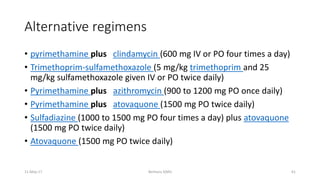
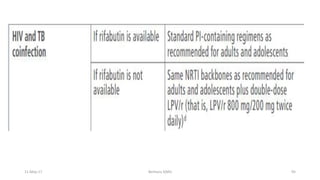
2) It provides details on various pulmonary, gastrointestinal and central nervous system OIs, including Pneumocystis jiroveci pneumonia, tuberculosis, and Mycobacterium avium complex.
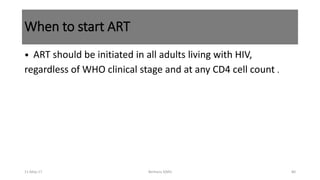
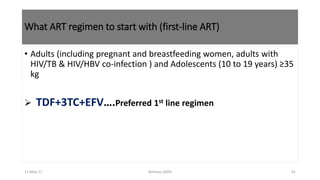
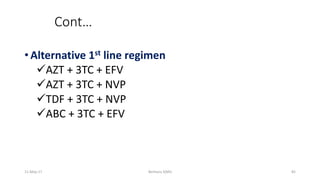
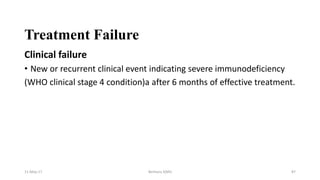
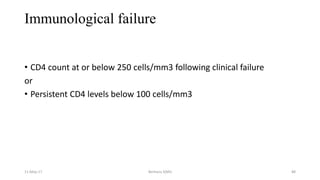
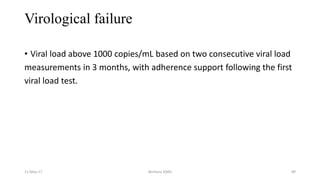
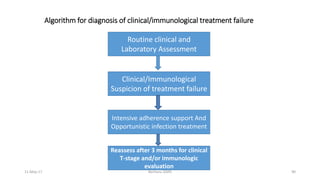
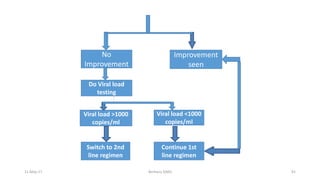
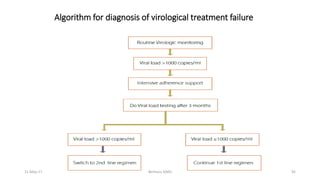
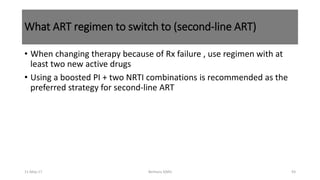
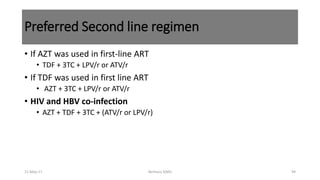
3) It also addresses when to initiate or switch ART regimens in cases of treatment failure.