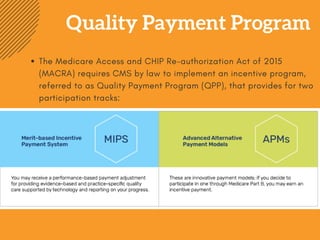
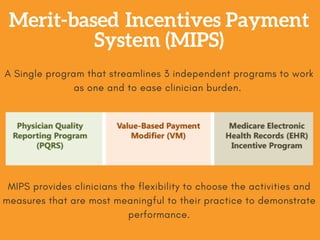
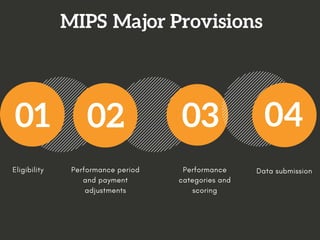
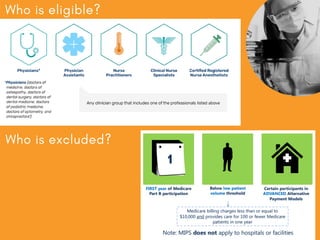
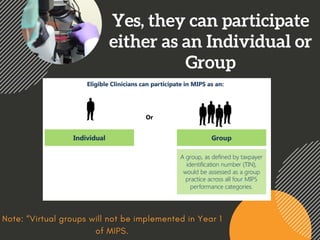
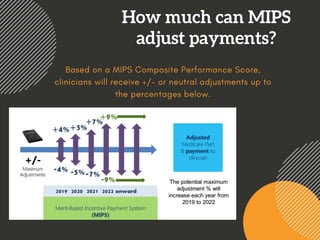
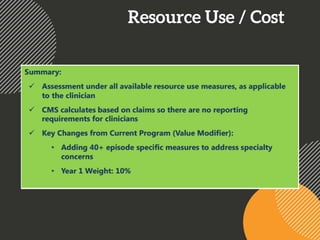
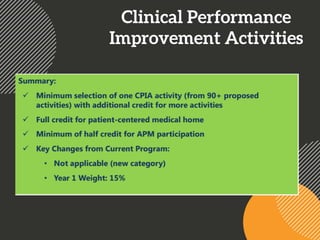
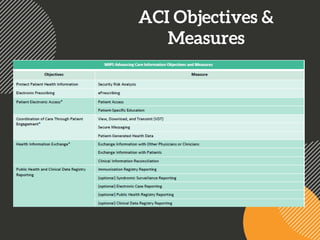
MIPS (Merit-based Incentive Payment System) is one of two participation tracks in the Quality Payment Program (QPP) established under MACRA. MIPS streamlines three previous programs into a single program to reduce clinician burden. It provides flexibility for clinicians to choose activities and measures most meaningful to their practice to demonstrate performance. MIPS performance is assessed based on four categories: Quality, Resource Use, Clinical Practice Improvement, and Advancing Care Information. Participation begins in 2017 and payment adjustments of up to +/- 4% will apply starting in 2019 based on a MIPS Composite Performance Score. Clinicians can participate as individuals or groups.