mental Health Nursing,MENTAL HEALTH TEAM OR MULTIDISCIPLINARY TEAM
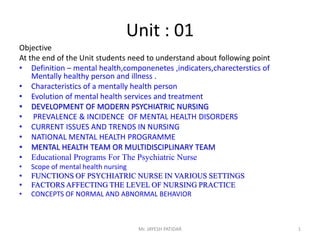
- 1. Unit : 01 Objective At the end of the Unit students need to understand about following point • Definition – mental health,componenetes ,indicaters,charecterstics of Mentally healthy person and illness . • Characteristics of a mentally health person • Evolution of mental health services and treatment • DEVELOPMENT OF MODERN PSYCHIATRIC NURSING • PREVALENCE & INCIDENCE OF MENTAL HEALTH DISORDERS • CURRENT ISSUES AND TRENDS IN NURSING • NATIONAL MENTAL HEALTH PROGRAMME • MENTAL HEALTH TEAM OR MULTIDISCIPLINARY TEAM • Educational Programs For The Psychiatric Nurse • Scope of mental health nursing • FUNCTIONS OF PSYCHIATRIC NURSE IN VARIOUS SETTINGS • FACTORS AFFECTING THE LEVEL OF NURSING PRACTICE • CONCEPTS OF NORMAL AND ABNORMAL BEHAVIOR Mr. JAYESH PATIDAR 1
- 2. Perspective of mental health& Mental health Nursing • Mental Health :- An adjustment of human being to the world & to each other with a maximum of effectiveness & happiness- Karl Menninger (1947) According APA – Simultaneous success at working ,loving & creating with the capacity for mature & flexible resolution of conflict between instincts,conscience,important other people & Reality Jayesh patidar 2
- 3. Components of mental health • The ability to accept self • The capacity to feel right towards others • The ability to fulfill life's task Criteria for mental health- -Adequate contact with reality -Control of thoughts and Imagination - Efficiency in work and play - Social acceptance - Health emotional life 3
- 4. Indicators of mental health • A positive attitude towards self • Growth ,devt.& the ability for self actualization • Integration • Autonomy • Perception of reality • Environmental mastery 4
- 5. Characteristics of a mentally health person • He has an ability to make an adjustments • Sense of personal worth ,feels worthwhile and important • Solve his problems largely by his own efforts & make his own decision • Sense of personal security &Feel secure in group ,Show understanding of other people problems and motives • Sense of responsibility 5
- 6. • Can give and accept love • Lives in world of reality rather than fantasy • Shows emotional maturity in his behavior & develop capacity to tolerate frustration & Disappointment in his daily life. • Developed philosophy of life that gives meaning and purpose to his daily activities. • Varity of interest &Generally lives a well balanced life of work ,rest and recreation. 6
- 7. Mental illness • Maladjustment in living • Mental & behavioral disorder are understood as clinically significant conditions characterized by alteration in thinking ,mood or behavior associated with personal distress and or Impaired functioning – WHO,2001 7
- 8. Characteristics of mental illness • Changes in ones thinking, memory ,perception, feeling & Judgment resulting in changes in talk and behavior which appeared to be deviant from previous personality or from the norms of community • These changes in behavior cause distress and suffering to the individual or others or both • Changes and the consequent distress causes disturbances in day to day activities ,work & relationship (Social & Vocational dysfunction ) 8
- 9. Evolution of mental health services and treatment • Pythagoras (580-510 BC) – Brain is the seat of intellectual activity • Hippocrates (460-370 BC)-Mental illness as hysteria, mania & Depression • Plato (420-347 BC)- Identify relation between mind and body • Asciepiades-father of psychiatry –Made use of simple hygiene ,measures,diet,,bath,massage in place of Mechanical restraints 9
- 10. • Greek were the first to study mental illness scientifically and separate the study of mind from religion .Aristotle ,a Greek philosopher ,emphasized on the release of repressed emotion for effective treatment.He suggested catharsis and music therapy for patients with melancholia . • Middle age – mentally ill were not considered as outcasts. but as people to be helped .one of the great figure during this time was St. Augustine ,believed that although God acted directly in human affairs, people were responsible for their own action. 10
- 11. • Renaissance in Europe(1300-1600AD )Saddest chapter – Demons were the cause of hallucinations, delusions and sexual activity & Treatment was torture & even death. 11
- 12. Some Important Milestone • 1773- first mental hospital in the US (Williamsburg,virginia) • 1793-Phillip Pinel removed chain • 1812 – First American textbook in psychiatry written by Benjamin Rush ,(Father of American Psychiatry ) • 1908- Clifford Beers,an ex- patient of a mental hospital wrote the book The mind that found itself based on his bitter experiennce(Founded American mental health association) 12
- 13. • 1912- Eugene Bleuler- Coined the term Schizophrenia • 1912 Indian Lunacy act was passed • 1927- Insulin shock treatment was used for schizophrenia • 1938- ECT Was used for psychoses. • 1946 –Bhore committee Recommendations five mental hospital were at Amritsar (1947),Hyderabad (1953),Srinagar (1958),Jamnagar (1960)&Delhi (1966).All india institue of mental health was set up at Bengaluru.(NIMHANS) 13
- 14. • 1949-Lithium was used mania • 1952- Chlorpromazine (Revolution of psychopharmacology) • 1963-Community mental health centre act was passed • 1978-Alma-ata declaration of Health for all BY 2000 A.D. posed a major challenge to Indian mental health professionals. • 1981-Community psychiatric centre was set up to experiment with primary mental health approach at Chandigarh & Sakalwara,Bengaluru. 14
- 15. • 1982-The centre council of Health ,India highest health policy making body accepted the National Mental health policy & brought out the National Mental health program . • 1987- Indian mental health act was passed.Govt India passed two acts, Mental health act 1987 & Person with disability act 1995 to protect the rights of persons with mental illness. 15
- 16. • 1990- Govt india formed an action group at delhi to pool the opinions of mental health experts about the national mental health program.NIMHANS Took leadership in orienting health programs of our country (Approaches) • Integration of mental heath care with general health care • School mental programs • Promotion of child mental health through Involvement of anganwadi(ICDS program) 16
- 17. • Crisis Intervention for suicide prevention • Halfway home for mentally ill individuals for social skill training ,vocational training • Education and involment of general public • Media material for public • Training for non professionals 1997 – National human rights commission prepared a plan of action for improving condition in mental hospital in the country & enhancing awareness of rights. 17
- 18. • 2001-Current situation analysis (CSA) was done to evolve a comprehensive plan of action to energize the NMHP. • Advanced centre for Ayurveda in mental health and neuroscience initiated research area like epilepsy ,M.R.,Schizophrenia • Advanced centre for yoga therapy and research at NIMHANS Started. • National human rights commission of India is mandated under section 12 of the protection of human Rights act 1993 to visit govt run mental hospital to study living conditions of inmates & make recommendations thereon. 18
- 19. • In 1997 project quality assurence in M.H.I to analyze condition generally prevalling 37 Govt run Mental hospital & Departments Finding – M.H .still being managed & administered custodial care .characters sized by prison -like stucture with high walls,watch towers,fenced wards & locked cells.MH like detention centre where person with mental illness kept caged in order to protect sociey from danger their existence poses. 19
- 20. • 2001 –On Augst 6th ,27 more mentally ill people died as they were tied to their beds when fire engulfed the thatched roof of the Moideen Badusha Mental home at Erwadi,Tamil Nadu state.Folloiwng tregedy ,national human right commision of india advised all chief minister to submitt a certificate stating no person with mental illness are kept chained ineither govt or private . • After this district wise survey of all registered & unregistered body purporting to offer mental health care & license to be granted on standards are maintained . • Govt implemented Distric mental health progrm which Incorporate the WHO community mental health care model.It focus on treatment availability at primary level,awareness ,,renovation,construction of Hospital. 20
- 21. • 2002-National survey of mental health Resources carried out by the Direcctorate General of health services ,Ministry of Health & Family well fare . • 2007- Under 11 five year plan ,centre of excellence in the field of mental health were established to upgrade & strengthen identified existing mental health hospitals for addressing acute manpower gap & provision of state of the art mental health care facilities in the long run. During this period 11 mental health institute were funded for developing as centre of excellence in mental health. 21
- 22. • 2008- WHO Mental health Gap action program was launched which aims at scaling up services for mental ,neurological & substance use disorders for countries with low &middle income. • 2013- WHO Launched Mental health action plan 2013-2020.Which identified imp.role of mental health in achieving health for all people.It stresses prevention of mental illness & aims to achieve equality through universal health coverage. 22
- 23. • 2013- Under 12th five plan govt of India integrated different componenent of national mental program with national rural health mission,namely school health,reproductive child health,&adolesent friendly clinics to reach out to the community in effective manner. • 2013- Mental health care Bill was introduced in Rajya sabha 0n 19 augst 2013.The bill abolished mental heath act 1987. • 2013- under central sector ,ministry of social justice & Empowerment launched Deendayal Disabled Rehabilitation Scheme & provided financial assistance to NGOs.for providing with disabilities & mental retardation including special school,half way homes,etc.National trust for wellfare of person with autism ,cerebral palsy,MR,&multiple disabilities various scheme for Rehabilitation such individual. • 2014- April 2011,govt of india constituted a policy group to recommended a mental health policy for the country.After due deliberations and Intense discussion group has recommended policy.Suggested policy has been duly considered by MOHAFW& Govt of India.National mental health policy is in accodance with intent of world health assembly resolution.This policy incorporates an integrated ,participatery rights & evidence based approach. 23
- 24. • World mental health day observed on 10 th oct every year. • Indian Psychiatric association- Profeshional body .Berkeley Hill of Ranchi Founded the Indian Association for mental hugiene in 1929.In 1935 indian division of the royal medicio psychological association was formed with effort of Banarasi Das.In1946 ,indian Psychiatric society was inaugereated. • Aims – promotion of metnal health & education,promote and advance subject pf psychiatry ,formulation&advise on the standards of education & traing in psychiatry,research.Indian journal of Psychiatry publishing. 24
- 25. • Indain Society of Psychiatric Nurses – started 1991 at NIMHANS,Bengaluru under guidance of Dr.K Reddemma.ISPN Publishing on journal Indian journal of Psychiatric nurses.1st conference child psychiatric nursing in2002. • Current issues,future perspects & challenges- India – Lack of clearly enunciated definition of the role of psychiatric nurses.Great emphasis should be given encourage M.sc.Nursing in Psychiatric nursing . • Need to offer more colleges in diploma in Psychiatric Nursing. • Psy nurse :pt ratio as per INC is 1:5 in Non teaching and 1:3 in Teaching hospital. • NMHP 1982 Recommended formation of Distric mental health team in order to decentralize mental health care at Distric level with 2 qualified psychiatric nurse and one psychiatrist. 25
- 26. • Analysis of 10 epidemiological studies shows prevalence rates as follow- • National prevalence rates for all mental disorder was 665.4/1000 population: with rural and urban rates of 64.4 and 66.4/1000 • Most widely prevalence disorder were observed to be depression and anxity.Urban morbidity rate was observed to be 2 per 1000,higher than rural morbidity rate.(Madhav MS 2001) • National prevalence rates for specific disorders • Schizophrenia – 2.3/1000 • Affective disorder – 31.2/1000 • Anxiety neurosis – 18.5/1000 • Hysteria – 4.1/1000 • Mental retardation – 4.2/1000 26
- 27. Prevalence &Incidence of mental health problems and disorder • Bhore committee – mental urban pt require institutional treatment would be 2 per 1000 in the country . All mental disorder – 73/1000 population, Rural 70.5 & urban73 • Schizophrenia 2.5/1000 • Affective disorder (Depression) 34/1000 • Anxiety neurosis – 16.5/1000 • Hysteria 3.3/1000 • Mental retardation 5.3/1000 • According health information of india 2005 mental morbidity rate is not less than 18-20/1000 and types of illness and their prevalence are very much the same as in other part of the world . 27
- 28. • According to community based epidemiological studies under WHO Mental health GAP Action program in India ,the estimated life time prevalence of mental disorder range from 12.2 to 48.6 % • MOHAFW suggests 6-7 %of India populations suffer from mental disorder with about 1 % suffering from severe mental disorder. while there in 10,000 people experience an episode of acute psychosis every year., about 25 % homeless. • Schizphrenia and bi – polar disorder are prevalent in about 200 cases per 10,000 people.burdon of these disorder is likely to increase to 15 % by 2020(Ghanshyam B,Nagarathiam S.India is failing the mentally ill as abuse continue. 28
- 29. • Common psychiatric illness encountered in a clinic of a General hospital are neurotic Disorder (anxity neurosis,OCD,reactive depression) • Psychosomatic disorder –(HTN,DM,Peptic ulcer,tension headache) • Functional psychosis – (Schizophrenia,mania,depression& organic psychosis) • Child guidance clinic – (MR,Conduct disorder,Hyperkineic syndrome,enuresis ) • Geriatric clinic – Depression,dementia,delusional disoreder • Psychosexual – Dhat syndrome,Premature ejacualation,erectile impotence ) • Prevalence 58.2per thousand which means that there are 5.7 crore people suffering from some sort of psychiatric disturbances .out of this 4 lakh have organic psychosis,26 lakh schizophrenia,1.2 crore affective psychosis:thus there are about 1.5 crore people suffering from severemental disorders.,Besides 12000 pt in Govt hospital. 29
- 30. • Mental Health act – Indian lunacy act ,Act4 of 1912,replaced the indian lunactic asylums act,act 36 of 1858.It was enacted to govern reception,detention and care of lunatics and their property and to consolidiate and amend the law relating lunacy. • Act was divided 4 parts & 8 chapters consisting 100 sections.The enactment of indian Lunancy act of 1912 was folowed by opening of many new asylums.an improvement in general conditions of asylums & increase in awareness regarding situation of asylums. • In 1946 Bhore committee submitted its recommendations .Indian psychiatric society ,established in jan1947,was quick to react to recommendations of committee .In Jan1949 an ad hoc drafting committee appointed which consisted of 3 distinguished psychiatrist.they prepared a draft bill called as the Indian mental Health act which was redrafted & finalize in 1950 and forwarded to govt of India .After 37 years mental health act 1987 passed was finally passed by Lok sabha ON 19 March 1987.Later govt of India issued orders that the act came into force effect from april1,1993 in all states and union Territories of India. It is an act to consolidate &amend law relating to the treatment & care of mentally ill persons ,to make better provision with respect to their property & affairs & for matters connected those with or incidental there to .the act divided in 10 chapter consisting 98 sections . 30
- 31. DEVELOPMENT OF MODERN PSYCHIATRIC NURSING Psychiatric nursing in general arose from the need for hospitals to provide socially acceptable levels of care. Some Important Milestones: 1840: Florence nightingale made an attempt to meet the needs of psychiatric patients with proper Hygiene, better food, light and ventilation and use of drugs. 31
- 32. 1872: First training school for nurses, based on the Nightingale system was established by the New England Hospital. 1882: First school to prepare nurses to care for the mentally ill was opened at McLean Hospital in Waverly. 1913: Johns Hopkins became the first school of nursing to include a fully developed course for psychiatric nursing in the curriculum. 32
- 33. 1943: Psychiatric nursing course was started for male nurses. 1956: One year post-certificate course in psychiatric nursing was started at NIMHANS, Bengaluru. 1960: The name ‘psychiatric nursing’ was changed to ‘psychiatric and mental health nursing’. 33
- 34. 1963: Journal of psychiatric nursing and mental health service was published. 1965: The Indian Nursing Council included psychiatric nursing as a compulsory course in the B.Sc Nursing program. 1967: The Trained Nurses Association of India (TNAI), formed a separate committee for psychiatric nursing. 34
- 35. 1973: Standards of Psychiatric and Mental health nursing practice were enunciated to provide a means of improving the quality of care. 1975: Psychiatric Nursing was offered as an elective subject in M.Sc Nursing at the Rajkumari Amrit Kaur College of Nursing, New Delhi. 1986: The Indian Nursing Council made psychiatric nursing a component of General Nursing and Midwifery course.American Psychiatric association established. 35
- 36. • 1990- Integration of neuroscience into holistic biopsychosocial practice of Psy.Nsg occurred. • Advances in understanding interrelationship of brain,behavior,emotion and cognition offered many new opportunities for psy.nurses.International council of nurses declared 1990 as the year of mental health nursing • 1991- Indian society of psychiatric nurses formed at NIMHNS ,Bengaluru • 1994- above mention changes led to revision of standards of psy & mental health nursing 36
- 37. • 1995- Journal of American Psychiatric Nurses Association established • 2000-Scope & standards of psy. Mental health clinical nursing was published by American nurses association. • 2003- American nurses association began certifying mental health practioshner. • 2010- ISPN published journal –Indian journal of Psychiatric Nurses. • Nurse role pt.advocacy,fiscal responsibility,profeshional collberation,Legal and ethical obligation. 37
- 38. CURRENT ISSUES AND TRENDS IN NURSING A psychiatric nurse faces various challenges because of changes in patient care approach. Some of these changes that affect her role are as follows: 38
- 39. Trends in health care Economic Changes Changes in illness orientation Changes in care delivery Information Technology Consumer empowerment 39
- 40. Deinstitutionalization Physicians shortage and gaps in service Demographic Changes Social Changes Mental Health Care Changes 40
- 41. TRENDS IN HEALTH CARE Increased mental health problems Provision for quality and comprehensive services Multi-disciplinary team approach Providing continuity of care Care is provided in alternative settings 41
- 42. ECONOMIC CHANGES Industrialization Urbanization Raised standard of living 42
- 43. CHANGES IN ILLNESS ORIENTATION Shift from illness to orientation (modification of style), specific to holistic, quantity of care to quality of care. 43
- 44. CHANGES IN CARE DELIVERY Care delivery is shifted from institutional services to community services, genetic services to counseling services, nurse patient relationship to nurse patient partnership. 44
- 45. CONSUMER EMPOWERMENT Increased consumer awareness Awareness of the community in early detection and treatment of mental illness as well as proper utilization of available psychiatric hospitals Patient are health care consumers demanding quality health care services at affordable cost with less restrictive and more humane rates 45
- 46. DEINSTITUTIONALIZATION Bringing mental health patients out of the hospital and shifting care to community 46
- 47. PHYSICIANS SHORTAGE AND GAPS IN SERVICE Physician shortage can provide the opportunity for new roles for example, nurse practitioner. In respect to gaps in services, nurses always meet the needs of people for whom services are not available, for example, home visiting nurse. 47
- 48. DEMOGRAPHIC CHANGES Type of family (increased number of nuclear families) Increasing number of the elderly group. 48
- 49. SOCIAL CHANGES The need for maintaining intergroup and intragroup loyalties Peer pressure. 49
- 50. MENTAL HEALTH CARE CHANGES Increased public awareness regarding mental health Need to maintain mental stability Increased mental health problems 50 Mr. jayesh patidar
- 51. Educational Programs For The Psychiatric Nurse • Diploma in Psychiatric Nursing (The first program was offered in 1956 at NIMHANS, Bangalore). • M.Sc in Psychiatric Nursing (The first program was offered in 1976 at Rajkumari Amrit Kauri College of Nursing, New Delhi). 51
- 52. • M. Phil. In Psychiatric Nursing (1990, M. G. University, Kottayam). • Doctorate in Psychiatric Nursing (offered at MAHE, Manipal; RAK College of Nursing, New Delhi; NIMHANS, Bangalore). • Short-term training programs for both the degree and diploma holders in nursing 52
- 53. Standards of Mental Health Nursing These standards are a means for improving the quality care for mentally ill people. They were enunciated by the American Nurses Association (ANA) in 1973. 53
- 54. Development of Code of Ethics This is very important for a psychiatric nurse as she takes up independent roles in psychotherapy, behaviour therapy, cognitive therapy, individual therapy, group therapy, maintains patient’s confidentiality, protects his rights and acts as patient’s advocate. 54
- 55. Legal Aspects in Psychiatric Nursing The practice of psychiatric nursing is influenced by law, particularly in its concern for the rights of patients and the quality of care they receive. The client’s right to refuse a particular treatment, protection from confinement, intentional torts, informed consent, confidentiality and record keeping are a few legal issues in which the nurse has to participate and gain quality knowledge. 55
- 56. Promotion of Research in Mental Health Nursing The nurse contributes to nursing and the mental health field through innovations in theory and practice and participation in research. 56
- 57. Cost-effective Nursing Care Studies need to be conducted to find out the viability in terms of cost involved in training a nurse and the quality of output in terms of nursing care rendered by her. 57
- 58. Focus of Care A psychiatric nurse has to focus care on certain target groups like the elderly, children, women, youth, mentally retarded and chronic mentally ill. 58
- 59. NATIONAL MENTAL HEALTH PROGRAMME INTRODUCTION: •Psychiatric symptoms are common in general population in both sides of the globe. •These symptoms - worry, tiredness, and sleepless nights affect more than half of the adults at some time. •While as many as one person in seven experiences some form of diagnosable neurotic disorder. 59
- 60. BURDEN OF DISEASE: •During the last two decades, many epidemiological studies have been conducted in India, which show that the prevalence of major psychiatric disorder is about the same all over the world. •The prevalence reported from these studies range from the population of 18 to 207 per 1000. • Most of these patients live in rural areas remote from any modern mental health facilities. 60
- 61. •A large number of adult patients (10.4 - 53%) coming to the general OPD are diagnosed mentally ill. (However, these patients are usually missed because either medical officer or general practitioner at the primary health care unit does not asked detailed mental health history). •Due to the under- diagnosis of these patients, unnecessary investigations and treatments are offered which heavily cost to the health providers. 61
- 62. National Mental Health Programme: The Government of India has launched the National Mental Health Programme (NMHP) in 1982, keeping in view the heavy burden of mental illness in the community, & the absolute inadequacy of mental health care infrastructure in the country to deal with it. 62
- 63. AIMS OF NMHP: 1. Prevention & treatment of mental & neurological disorders & associated disabilities. 2. Use of mental health technology to improve general health services. 3. Application of mental health principles in total national development to improve quality of life. 63
- 64. OBJECTIVES OF NMHP: 1. To ensure availability and accessibility of minimum mental health care for all in the foreseeable future, particularly to the most vulnerable and underprivileged sections of population. 2. To encourage application of mental health knowledge in general health care and in social development. 3. To promote community participation in the mental health services development and to stimulate efforts towards self-help in the community. 64
- 65. STRATEGIES OF NMHP: 1. Integration mental health with primary health care through the NMHP; 2. Provision of tertiary care institutions for treatment of mental disorders; 3. Eradicating stigmatization of mentally ill patients and protecting their rights through regulatory institutions like the Central Mental Health Authority, and State Mental health Authority. 65
- 66. APPROACHES OF NMHP: Integration of mental health care services with the existing general health services. Utilization of the existing infrastructure of health services and also deliver the minimum mental health care services. Provision of appropriate task oriented training to the existing health staff. Linkage of mental health services with ht existing community development programme. 66
- 68. I. Treatment: Multiple levels A. • Village and Sub-centre level B. • MO of Primary Health Centre C. • District Hospital D. • Mental Hospitals and teaching psychiatric units 68
- 69. A. Village and Sub-centre level: Multipurpose workers (MPW) and Health Supervisors (HS), under the supervision of Medical Officer (MO) to be trained for: •Management of Psychiatric emergencies •Administration and supervision of maintenance treatment for chronic psychiatric disorders. 69
- 70. •Diagnosis and management of grandmal epilepsy, especially in children. •Liaison with local school teachers and parents regarding mental retardation and behavioral problems in children. •Counseling problems related to alcohol and drug abuse. 70
- 71. B. MO of Primary Health Centre (PHC) aided by HS, to be trained for: •Supervision of MPW’s performance. •Elementary diagnosis. •Treatment of functional psychosis. •Treatment of uncomplicated cases of psychiatric disorders associated with physical diseases. •Management of uncomplicated psychosocial problems. •Epidemiological surveillance of mental morbidity. 71
- 72. C. District Hospital: It was recognized that there should be at least one psychiatrist attached to every district hospital as an integral part of the district hospital services. The hospital should have 30-50 psychiatric beds. The psychiatrist in a district hospital was envisaged to devote only a part of his time to clinical care and a greater part in training and supervision of non-specialist health workers. 72
- 73. D. Mental Hospitals and teaching psychiatric units: Major activities of these higher centers of psychiatric care include: •Help in care of ‘difficult’ cases. •Teaching. •Specialized facilities like, occupational therapy units, psychotherapy, counseling and behavioral therapy. 73
- 74. II. Rehabilitation: The components of this sub-program include treatment of epileptics and psychotics at the community level and development of rehabilitation centers at both the district level and higher referral centers. 74
- 75. III. Prevention: The prevention component is to be community based, with initial focus on prevention and control of alcohol-related problems. Later on, problems like addictions, juvenile delinquency and acute adjustment problems like suicidal attempts are to be addressed. 75
- 76. MENTAL HEALTH TEAM OR MULTIDISCIPLINARY TEAM: Multidisciplinary approach refers to collaboration between members of different disciplines who provide specific services to the patient. The multidisciplinary team includes: 76
- 77. MENTAL HEALTH TEAM 1. PSYCHIATRIST 2. PSYCHIATRIC NURSE 3. CLINICAL PSYCHOLOGIST 4. PSYCHIATRIC SOCIAL WORKER 5. OCCUPATIONAL THERAPIST OR ACTIVITY THERAPIST 6. PHARMACIST AND DIETICIAN 7. COUNSELOR 77
- 78. 1. PSYCHIATRIST: A psychiatrist is a medical doctor with a special training in psychiatry. He is accountable for the medical diagnosis and treatment of patient. Other important functions are: •Admitting the patient into acute care setting. •Prescribing and monitoring psychopharmacologic agents. 78
- 79. •Administering ECT. •Conducting individual and family therapy. •Participating in interdisciplinary team meetings. •Owing to their legal power to prescribe and to write orders, psychiatrists often function as leaders of the team. 79
- 80. 2. PSYCHIATRIC NURSE: A psychiatric nurse is a registered nurse with specialized training in the care and treatment of psychiatric patients; she may have a Diploma, M.Sc, M.Phil or PhD in psychiatric nursing. She is accountable for the bio-psychosocial nursing care of patients and their milieu. Other functions include: 80
- 81. •Administering and monitoring medications. •Assisting in numerous psychiatric and physical treatments. •Participate in interdisciplinary team meetings. •Teach patients and families. •Take responsibility for patient’s records. •Act as patient’s advocate. •Interact with patient’s significant others. 81
- 82. 3. CLINICAL PSYCHOLOGIST: A clinical psychologist should have a Masters Degree in Psychology or Ph.D degree in clinical psychology with a specialized training in mental health settings. He is accountable for psychological assessments, testings, and treatments. He offers direct services such as individual, family or marital therapies. 82
- 83. 4. PSYCHIATRIC SOCIAL WORKER: A psychiatric social worker have a Masters Degree in Social Work or Ph.D degree with a specialized training in mental health settings. He is accountable for family case work and community placement of patients. He conducts group therapy sessions. He emphasizes intervention with the patient in social environment in which he will live. 83
- 84. 5. OCCUPATIONAL THERAPIST OR AN ACTIVITY THERAPIST: An occupational therapist or an activity therapist is accountable for recreational, occupational and activity programs. He assists the patients to gain skills that help them cope more effectively to gain or retain employment, to use leisure time. 84
- 85. 6. PHARMACIST AND DIETICIAN 85
- 86. 7. COUNSELOR: A counselor provides basic supportive counseling and assists in psycho educational and recreational activities. 86
- 87. SCOPE OF MENTAL HEALTH NURSING The areas of concern for the psychiatric mental health nurse include a wide range of actual or potential mental health problems, such as emotional stress or crisis, self concept changes, development issues, physical symptoms that occur with psychological changes, and symptom management of patient with mental disorders. 87
- 88. To understand the problem and select an appropriate intervention, integration of knowledge from the biological, psychological and social domain necessary. Today the scope of mental health nursing is not restricted within the confines of the bedside nursing care. A mental health nurse needs to be skilled and clinically competent, sensitive to the social environment, the advocacy needs of the patients and their families as well as be aware of the legal and ethical dilemmas. 88
- 89. ROLE OF A PSYCHIATRIC NURSE Primary mental health nursing Collaborative psychiatric nursing practice Clinical Nurse Specialist (CNS) Nurse psychotherapist Psychiatric nurse educator Psychosocial rehabilitation nursing Child psychiatric nursing Gerontological and geriatric nursing Deaddiction nursing Neuropsychiatric nursing Community mental health nursing 89
- 90. Primary Mental Health Nursing Psychiatric nurses are moving into the domain of primary care and working with other nurses and physicians to diagnose and treat psychiatric illness in patients with somatic complaints. Cardiovascular, gynecological, respiratory, gastrointestinal and family practice settings are appropriate for assessing patients for anxiety, depression and substance abuse disorders. 90
- 91. Collaborative Psychiatric Nursing Practice Patients who are having difficulty being stabilized on their medications or who have co- morbid medical illnesses are seen in a psychiatric nursing clinic where nurses and physicians collaborate to provide high quality patient care. 91
- 92. Clinical Nurse Specialist (CNS) The Clinical Nurse Specialist provides consultative services to nursing personnel. She attends clinical teaching programs, demonstrates therapies, conducts in-service education programs, initiates and participates in curriculum revision/changes and nursing research. 92
- 93. Nurse Psychotherapist The psychiatric nurse can take up psychotherapy roles as in individual therapy, group therapy, counseling etc. 93
- 94. Psychiatric Nurse Educator The main function of psychiatric nurse educator is planning and changing the curriculum according to the needs of the society and learner. The number of nurses in the field of teaching psychiatric nursing needs to be enhanced. This is a big challenge for nursing curriculum planners. 94
- 95. Psychosocial Rehabilitation Nursing It is concerned with helping people with chronic mental illness to lead more independent and satisfactory lives in the community. 95
- 96. Child Psychiatric Nursing In child psychiatric nursing the nurse identifies the emotional and behavioral problems of the children and provides comprehensive care. 96
- 97. Gerontological and geriatric nursing Gerontological nursing provides emotional support to those people who have retired from services, who have no financial sources and helps them in understanding the situation and developing new coping mechanisms. Geriatric nursing is expanding the psychiatric nursing practice to aged people who have been affected by emotional and behavioral disorders such as dementia, chronic schizophrenia, delirium etc. 97
- 98. Deaddiction Nursing A psychiatric nurse in these units, identifies psychosocial problems and maintaining factors in addicts. She also provides various therapies to the addicts and their family members. 98
- 99. Neuropsychiatric Nursing Psychiatric nursing practice is extended to patients who are suffering from neuro-psychiatric disorders such as dementia, epilepsy, brain tumour, head injury with behavioural problems, HIV infection with behavioural problems etc. 99
- 100. Community Mental Health Nursing It is the application of knowledge of psychiatric nursing in preventing mental illness, promoting and maintaining mental health of the people. It includes early diagnosis, appropriate referrals, care and rehabilitation of mentally ill people. 100
- 101. FUNCTIONS OF PSYCHIATRIC NURSE IN VARIOUS SETTINGS 1. Inpatient Psychiatric ward 2. Psychiatric outpatient department 3. ECT training centre 4. Psychotherapy unit 5. Day care centers or Day hospitals 6. Family therapy units 101
- 102. 7. Child psychiatric ward 8. Home settings 9. Community mental health centers 10. Hospice care centers 11. Emergency departments 12. Medical inpatient wards 13. Industrial medical centers 14. Hospitals for criminal insane, jails and prisons102
- 103. INPATIENT PSYCHIATRIC WARD: •Provide safe environment •Perform psychosocial, high risk and physical assessment •Promotion of self care activities •Medication management •Observing and documenting the patient’s behavior •Help in decision making and assuming the responsibility of life 103
- 104. •Providing feed back •Participation in various therapies •Psycho education •Counseling •Social skills and stress management techniques •Discharge, referral and follow up care •Supervision of subordinates •Cleanliness 104
- 105. PSYCHIATRIC OUTPATIENT DEPARTMENT: •Clinical assessment •Psychometric assessment •Psychotherapy •Counseling •Conducting group therapy •Psycho education 105
- 106. ECT TRAINING CENTRE: •Teaching •Preparation for ECT •Providing care •Assist with post treatment •Providing reassurance •Psycho education regarding ECT 106
- 107. PSYCHOTHERAPY UNIT; •Establishing therapeutic nurse patient relationship •Assisting the patient •Providing opportunities to practice new skills •Reinforcing appropriate behavior •Emotional support 107
- 108. DAY CARE CENTERS OR DAY HOSPITALS: •Clinical assessment •Observing and documenting patient behavior •Medication management •Teaching social skills •Counseling •Psycho education •Occupational and recreational therapy 108
- 109. FAMILY THERAPY UNITS: •Assessing the individual and family needs •Facilitation of a family •Promote adaptive family functioning •Psycho education 109
- 110. CHILD PSYCHIATRIC WARD: •Assessing biological and psychological need of the child •Determine the child’s strengths and limitations •Monitor the child’s developmental levels •Provide a safe therapeutic environment •Teaching self care skills •Genetic counseling •Psycho education •Medication management •Emotional support •Participate in various therapies 110
- 111. HOME SETTINGS: •Assessment of symptoms •Teaching •Stress management •Medication management •Case manager •Appropriate referrals to community agency •Venipuncture for lab analysis •Supportive counseling and psychotherapy •Promotion of mental health and prevention of mental illness 111
- 112. COMMUNITY MENTAL HEALTH CENTERS: •Identification of patient •Refer the patient to hospitals •Home visit •Follow up care •Conducting public awareness programme •Training of paraprofessionals •Management of resources planning and co-ordination 112
- 113. HOSPICE CARE CENTERS: • Helping cancer or terminally ill individuals •Providing supportive psychotherapy •Provide support groups for families of terminally ill 113
- 114. EMERGENCY DEPARTMENTS: •Crisis intervention during natural disasters •Obstetric nursing centers •Helping the mother in labor •Providing support to bereaved parents 114
- 115. MEDICAL INPATIENT WARDS: • Psychosocial intervention for chronic illnesses with major psychological effects 115
- 116. INDUSTRIAL MEDICAL CENTERS: •Implementing and participating in industrial substance abuse programs for employees •Providing crisis intervention •Stress management 116
- 117. HOSPITALS FOR CRIMINAL INSANE, JAILS AND PRISONS: • Medication management •Promote coping skills •Diagnose and treat psychiatric disorders •Psychotherapy •Assessment for potential for violence •Review of police reports 117
- 118. FACTORS AFFECTING THE LEVEL OF NURSING PRACTICE The level at which psychiatric nurses practice is determined by various factors such as: •Nurse Practice Acts (Laws) •Professional Practice Standards •Educational qualifications and experience •Health care organization philosophy •Self motivation and personal initiatives 118
- 119. Nurse Practice Acts (Laws): Nurse practice acts regulate entry into the profession and define the legal limits of nursing practice that must be adhered to by all nurses. Nurses must be familiar with the nurse practice act of their state and limit their practice. 119
- 120. Professional Practice Standards: Professional Practice Standards define nursing practice and performance; first developed by the ANA in 1973 and recently revised in 2000. 120
- 121. Educational qualifications and experience Nurses’ qualifications include education, work experiences and certification status which determine the level of practice. 121
- 122. Health care organization philosophy A Health care organization philosophy of mental health and mental illness and its approach towards treatment help to share the expectations of both the nurses and patient. 122
- 123. CONCEPTS OF NORMALAND ABNORMAL BEHAVIOR Psychiatry as evident from the above is concerned with abnormal behavior in its broadest sense, but defining the concepts of normal and abnormal behavior as such has been found to be difficult. These concepts are much under the influence of socio-cultural factors. Several models have been put forward in order to explain the concept of normal and abnormal behavior. Some of these are: 123
- 125. MEDICAL MODEL: •Medical model considers organic pathology as the definite cause for mental disorder. • According to this model abnormal people are the ones who have disturbances in thought, perception and psychomotor activities. •The normal are the ones who are free from these disturbances. 125
- 126. STATISTICAL MODEL: •It involves the analysis of responses on a test or a questionnaire or observations of some particular behavioral variables. •The degree of deviation from the standard norms arrived at a statistically, characterizes the degree of abnormality. •Statistically normal mental health falls within two standard deviations (SDs) of the normal distribution curve. 126
- 127. SOCIO-CULTURAL MODEL: The beliefs, norms, taboos and values of a society have to be accepted and adopted by individuals. •Breaking any of these would be considered as abnormal. •Normalcy is defined in context with social norms prescribed by the culture. •Thus cultural background has to be taken into account when distinguishing between normal and abnormal behavior. 127
- 128. BEHAVIOR MODEL: •Behavior that is adaptive, is normal, maladaptive is abnormal. •Abnormal behavior is a set of faulty behaviors acquired through learning. 128