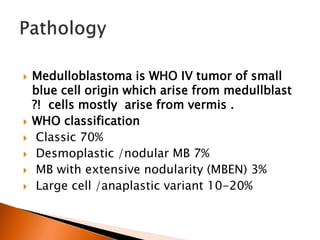
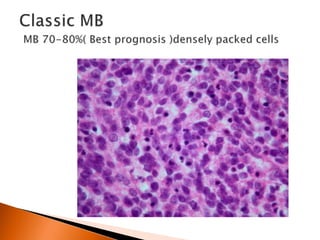
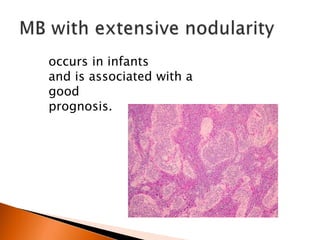
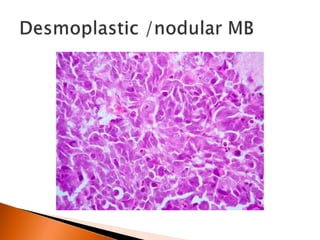
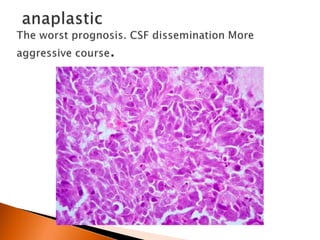
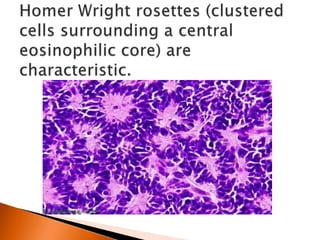
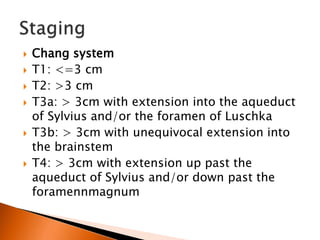
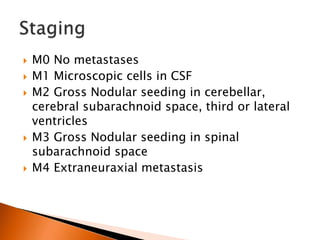
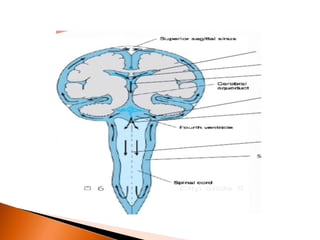
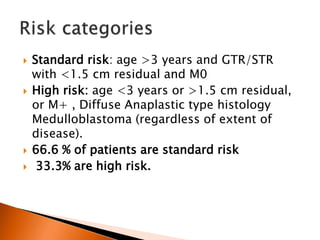
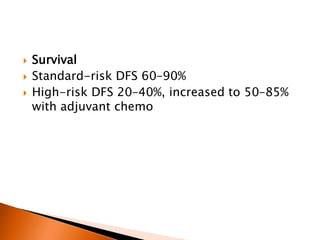
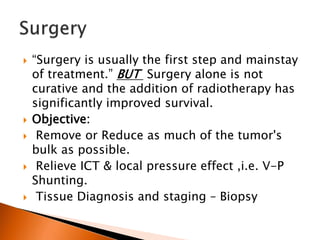
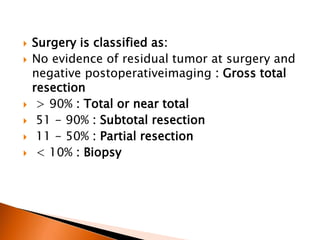
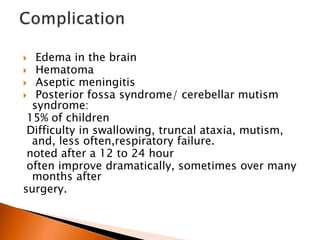
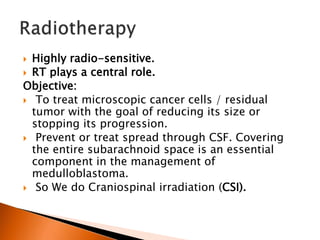
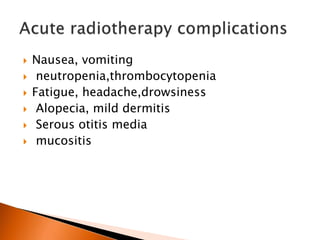
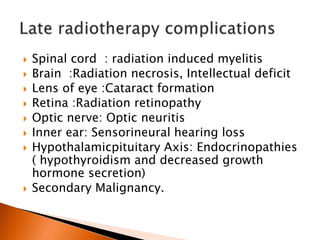
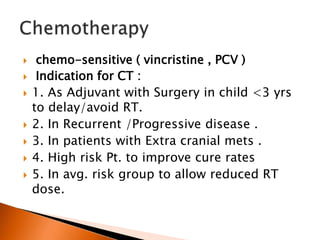
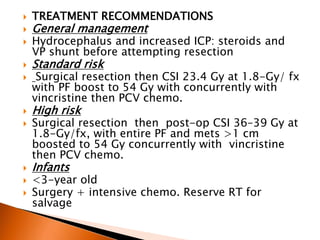
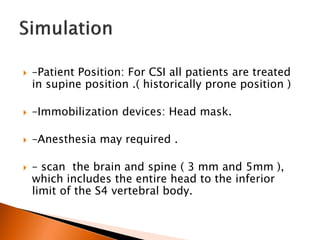
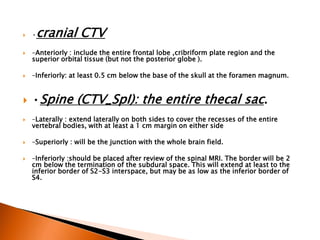
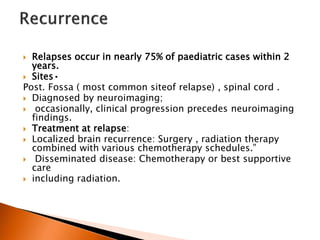
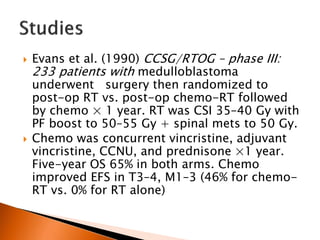
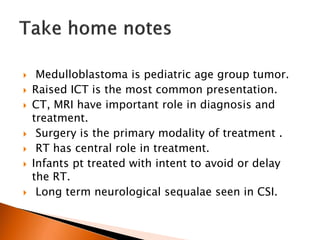
The document discusses medulloblastoma, a type of brain tumor that occurs most often in children. It arises from primitive cells located in the cerebellum. Key points include that surgery is usually the first treatment, but radiation therapy plays a central role in improving survival. Treatment may involve craniospinal irradiation with a boost to the tumor site. Prognosis depends on factors like age and extent of disease. Long term side effects can include neurological and endocrine issues due to radiation therapy.