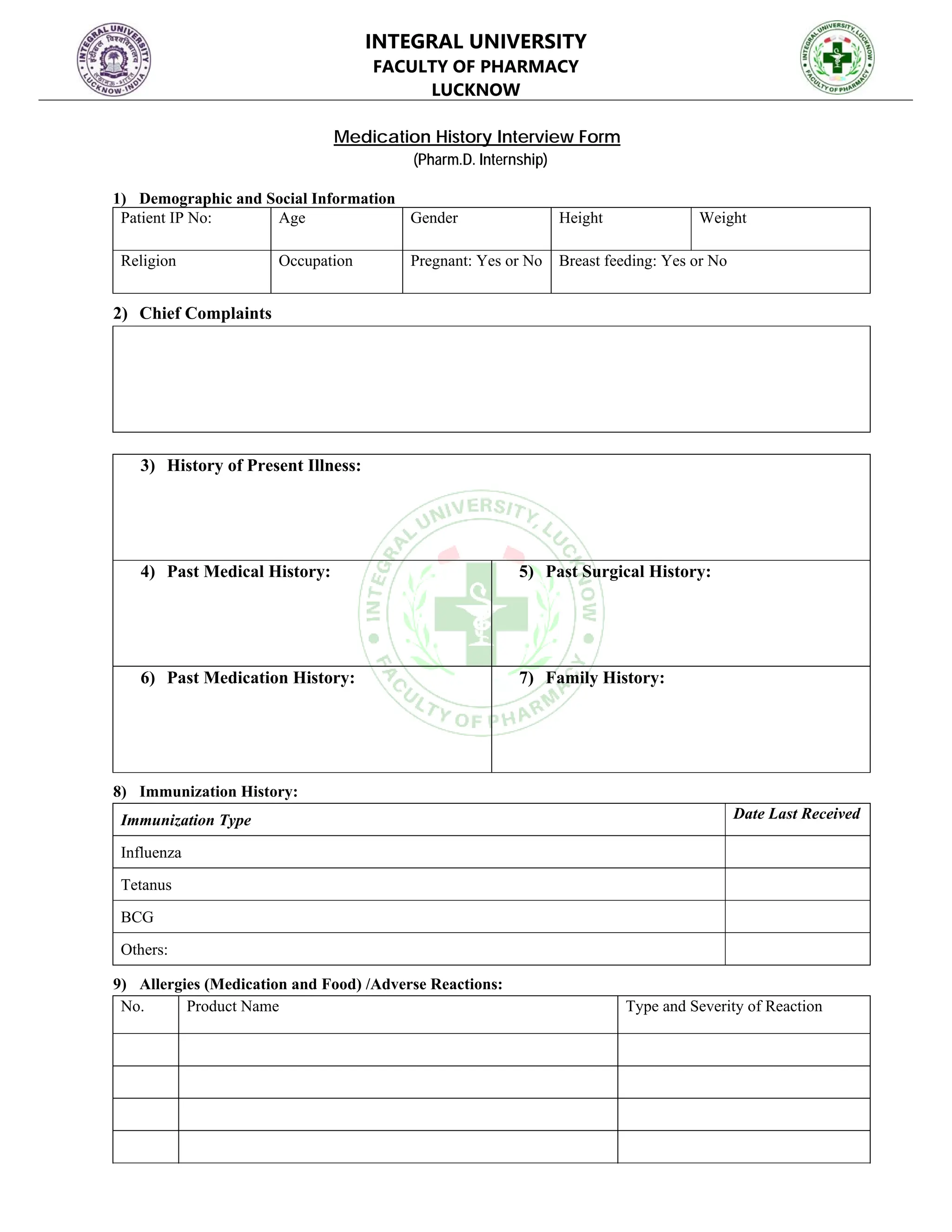
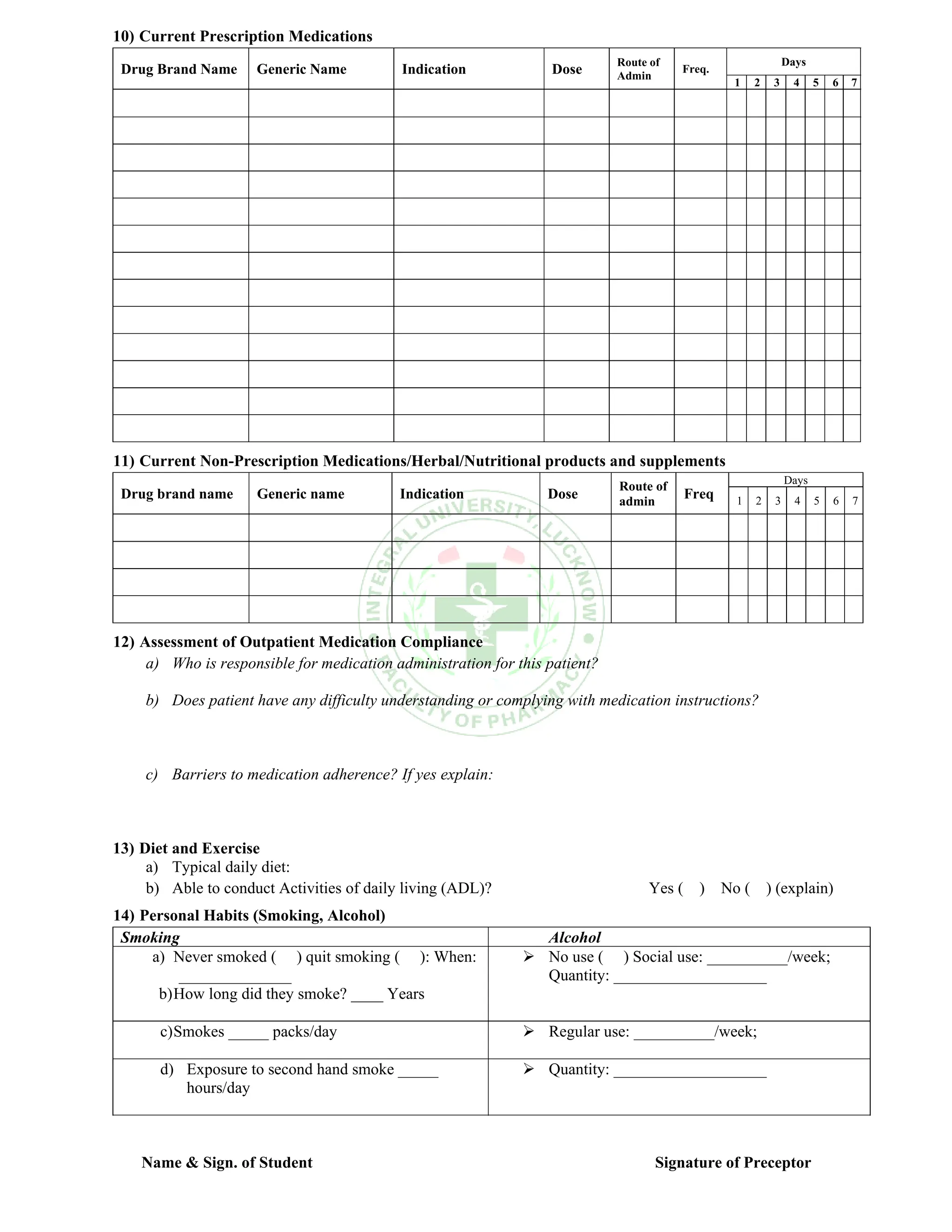
The document is a medication history interview form for Pharm.D. internships at Integral University Faculty of Pharmacy, detailing sections to collect demographic data, chief complaints, medical history, current medications, and patient compliance. It includes assessments on allergies, immunizations, personal habits, diet, and exercise. Finally, it aims to evaluate the patient's understanding and compliance with medication instructions.