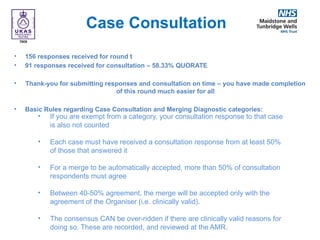
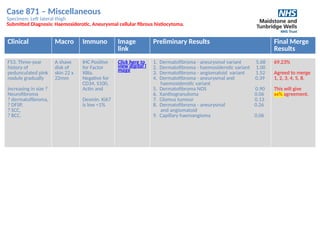
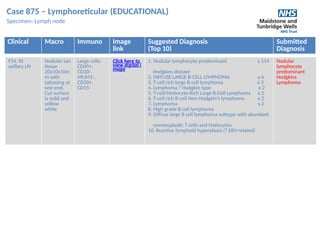
The document outlines a meeting for the South East England General Histopathology EQA Scheme held on November 30, 2022, covering case discussions and preliminary score reviews of various specimens. The agenda included introductions, a review of cases 865-874, and discussions on merging decisions based on participant responses. Participants were reminded of the meeting's educational purpose and the process for providing feedback and earning CPD points.