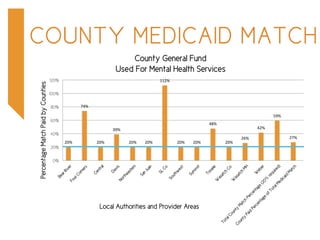
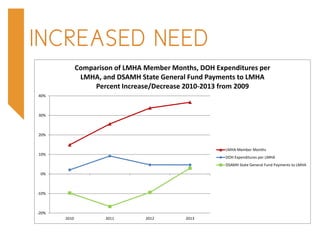
The report outlines the financial structures and challenges faced by local mental health authorities in Utah, particularly regarding Medicaid funding and county matching requirements. It highlights the shift from a fee-for-service system to a capitated Medicaid system, the resultant savings, and the need for ongoing Medicaid match funding to support behavioral health services. There is a call for an additional $6.4 million in ongoing Medicaid match funds for the 2016 legislative session to address growing service demands.